DEFINITION
- Plasma potassium level <3.5 mmol/L or below normal level defined by local laboratory
- Symptoms may occur if potassium level <3 mmol/L
- May be a late sign of total body potassium depletion due to mobilisation of intracellular potassium stores
SYMPTOMS AND SIGNS
- Muscle weakness and paralysis
- Arrhythmias (premature atrial and ventricular beats, sinus bradycardia, paroxysmal atrial or junctional tachycardia, atrioventricular block, and ventricular tachycardia or fibrillation)
- ECG changes
- increased amplitude and width of P wave
- prolongation of PR interval
- T wave flattening and inversion
- ST depression
- prominent U waves (best seen in precordial leads)
- apparent long QT interval due to fusion of T and U waves

T wave inversion and prominent U wave
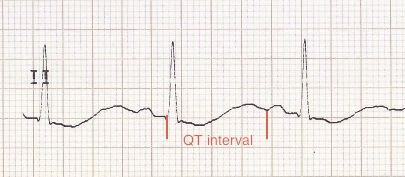
Apparently long QT interval (actually T-U fusion)
CAUSES
- Low oral intake/potassium concentration in IV fluids
- Renal loss
- diuretics
- bicarbonate administration
- renal tubular acidosis
- inherited salt-losing tubulopathies e.g. Bartter syndrome
- Diarrhoea (Note: potassium content of lower GI loss is greater than upper GI loss)
- Alkalosis (approximately 0.4 mmol/L fall in potassium for every 0.1 unit rise in pH)
- Insulin administration
- Salbutamol administration (high-dose, nebuliser/IV)
- Liposomal-amphotericin (prolonged use)
- Doxapram
- Increased mineralocorticoid activity, due to:
- hypovolaemia
- 11- beta-hydroxylase deficiency (rarer form of congenital adrenal hyperplasia – presents with virilization, hypertension, and hypokalemia)
- primary hyperaldosteronism
INVESTIGATIONS
- Confirm value on venous laboratory sample (Note: ‘normal’ value on capillary sample may be falsely reassuring if sample has haemolysed and true value is lower)
- ECG
- Cardiac monitor, if ECG changes present
- Mild hypokalaemia (serum level 3–3.5 mmol/L) does not require investigation
- if hypokalaemia persists or >2 mmol/kg/day maintenance is required – investigate as for significant hypokalaemia (below)
- If significant hypokalaemia (serum level <3 mmol/L) and no obvious cause check:
- acid/base balance and bicarbonate level on blood gas
- urinary potassium level. Level >20 mmol/L suggests excess renal potassium losses
- if baby is hypertensive, measure plasma renin and aldosterone
- If hypokalaemia not responding well to replacement, check magnesium level
IMMEDIATE MANAGEMENT
- Supplement feeds/fluids
- normal maintenance potassium requirement is 2 mmol/kg/day
- higher amounts will be needed to correct hypokalaemia
- Review medications
- if baby is on insulin infusion, consider stopping
Symptomatic babies
- Give rapid potassium supplementation
- 'Strong potassium' solution
- contains 20 mmol/10 mL
- must be diluted at least 50-fold with sodium chloride 0.9% or a mixture of sodium chloride 0.9% in glucose before administration
- maximal peripheral concentration 40 mmol/L (1 mmol in 25 mL)
- maximal central concentration 80 mmol/L (1 mmol in 12.5 mL)
- rate 0.2 mmol/kg/hr (maximum 0.5 mmol/kg/hr if severe potassium depletion)
- Continuous cardiac monitoring necessary
- Recheck potassium 2–4 hr and assess need for continuing infusion
Asymptomatic babies
- Potassium replacement given according to how baby is being fed:
- orally fed babies
- oral supplement e.g. potassium chloride 1 mmol/kg 12-hrly. Titrate dose according to response
- babies on IV fluids
- add potassium chloride 3−5 mmol/kg/day to IV fluid, depending on electrolyte levels and titrate according to response
- babies receiving parenteral nutrition (PN)
- increase potassium content of the PN to 3–5 mmol/kg/day
- if modified PN not available, run separate potassium infusion 3–5 mmol/kg/day alongside current PN
- orally fed babies
SUBSEQUENT MANAGEMENT
- Monitor potassium levels according to clinical need:
- well babies receiving oral potassium check level once to twice weekly
- well babies on IV fluids or PN with mild hypokalaemia (potassium 3–3.5 mmol/L) check level daily
- check more frequently if:
- significant hypokalaemia (serum level <3 mmol/L)
- symptomatic hypokalaemia
- concentrations of potassium >5 mmol/kg/day are being given
- Once plasma/serum potassium level is in normal range, continue potassium supplementation to allow replenishment of total body potassium (intracellular) stores:
- orally fed – continue for a further week
- IV fluids/PN − reduce potassium to 2 mmol/kg/day as maintenance
- recheck potassium level following these changes to ensure hypokalaemia does not recur
Date updated: 2024-01-11