HAND HYGIENE
- Describes decontamination of hands using soap and water, antiseptic wash or alcohol hand rub solution
- Good hand hygiene is the most effective way to prevent spread of infection
- Use this safe method of working at all times to protect staff, patients and others from infection
- All practitioners are personally accountable for their hand hygiene practice, and for the decontamination of all re-usable equipment that they touch and use in clinical practice
ASSESSMENT OF NEED TO DECONTAMINATE HANDS
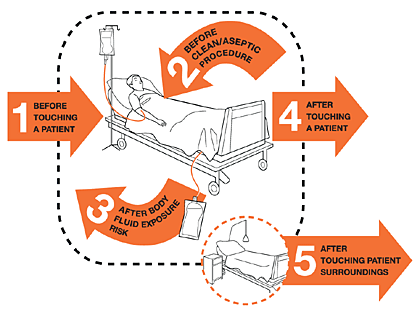
Hands must be decontaminated at critical points before, during and after patient care to prevent cross-infection of micro-organisms - see World Health Organization (WHO) 5 moments for hand hygiene
- Hand decontamination must be carried out at the following 5 moments of care regardless of whether or not gloves have been worn
- before touching a patient
- before and after aseptic non-touch technique (ANTT)/aseptic procedure
- after body fluid exposure
- after touching a patient
- after touching patient surroundings
Figure 1: Five moments for hand hygiene
- Hands must also be decontaminated
- on arrival at and before leaving ward/department
- after visiting the toilet
- before serving/preparing food or drinks
- after any activity or contact that potentially results in hands becoming contaminated
- on entering and leaving an isolation cubicle
- after removing personal protective equipment
CHOICE OF HAND HYGIENE PREPARATIONS
- Alcohol hand rub is an effective method of hand decontamination on visibly clean hands but is not recommended when hands are visibly dirty
Alcohol hand rub alone must not be used after caring for patients (or their equipment/environment) with suspected or known infectious diarrhoea e.g. C. difficile or Norovirus, regardless of whether gloves are worn
- Hand washing with liquid soap and water removes dirt, organic matter and transient flora by mechanical action, and is to be used:
- when hands are visibly dirty/visibly soiled with body fluids or other organic matter
- when caring for patients with:
- suspected or confirmed diarrhoea and/or vomiting
- C. difficile/Norovirus and during outbreaks of these organisms on wards/in bays
- after several consecutive applications of alcohol hand rub
- after visiting the toilet
- Liquid soap alone does not provide sufficient hand disinfection before invasive procedures and surgery
DRESS CODE
- Bare below elbow for all staff working within clinical areas (e.g. no sleeves below elbow, no wrist watches, wrist jewellery or plaster casts/wrist splints)
- Do not wear false nails, nail extensions, gel nails or nail varnish
- Keep nails short and clean
- No stoned rings (acceptable to wear a plain wedding band)
- Long hair tied back or up
PERSONAL PROTECTIVE EQUIPMENT (PPE)
Aprons
- <2 metres of child with respiratory tract infection
- Contact with infectious materials or equipment anticipated
- Using hazardous chemicals
- ANTT – see below
Gloves (non–sterile)
- Contact with respiratory secretions or other infectious material of contaminated surfaces
- ANTT – see below
- Single patient use; new gloves and apron for every procedure
- Take gloves and apron off at point of use and clean hands
- Do not carry gloves in your pocket
- Do not use alcohol hand rub on gloves
Remove gloves and aprons as soon as clinical activity completed,
before touching pens, notes, phone, computer etc.
Sterile gloves and gown
- For central venous line (CVL) including peripheral long line (PICC)
- Sterile gloves for ANTT if touching key parts/key sites
Masks
- Surgical face mask
- <2 metres of child with respiratory tract infection
- FFP3 mask (fit-tested)
- aerosol generating procedure (e.g. intubation, CPAP, HFNC, suctioning of lower respiratory tract, bag mask ventilation) with respiratory tract infection and when advised by infection prevention team
- in conjunction with eye protection when increased risk of splashing of body fluids into eyes/nose/mouth
Eye protection
- <2 metres of child with persistent coughing or sneezing
- When increased risk of splashing of body fluids in to eyes
- If increased risk of organism transmitted through conjunctiva (e.g. SARS CoV-2)
SURGICAL ANTT
- See local ANTT guidelines
Definition
- Essential procedure aimed at protecting patients from infection during invasive procedures
- Achieved by minimising presence of pathogenic micro-organisms as is practically possible
- Specific type of aseptic technique with a unique theory and practice framework, providing core principles for safe aseptic technique and a standardised approach to assessing and applying safe aseptic technique to any invasive clinical procedure
- Do not touch and protect ‘key parts’ or ‘key sites’ e.g. use caps and covers for end of syringes/needles
Preparation phase
- Decontaminate hands
- Decontaminate tray/trolley using Trust approved disinfectant
- Clean hands
- PPE (as above)
- Prepare and assemble equipment using a non-touch technique. Protect key parts at all times by not touching
- Remove gloves and decontaminate hands
Patient phase
- Decontaminate hands at point of care
- Apply appropriate PPE. Non-sterile gloves if not touching key parts (e.g. IV drug administration, venepuncture/cannulation), sterile gloves if touching key parts (e.g. urinary catheterisation, central line/PICC insertion)
- Prepare all equipment using a non-touch technique, protecting key parts at all times by not touching them
- Decontaminate key parts/key sites using single use chlorhexidine 2% in alcohol 70% (SEPP/FREPP or ChloraPrep® 3 mL) and allow drying for 30 sec
- Perform procedure, ensuring protection of key parts/sites at all times
Decontamination phase
- Dispose of sharps into sharps box immediately at point of use
- Remove PPE at bedside
- Dispose of all equipment as clinical waste in nearest clinical waste bin, return equipment to clinical room ensuring it is cleaned with detergent wipes
- Decontaminate hands
Date updated: 2024-01-15