RECOGNITION AND ASSESSMENT
Definition
- Decreased mineralisation of bones due to deficient phosphate (PO4), calcium (Ca) or vitamin D in preterm babies
- Also known as osteopenia of prematurity
Causes
- Inadequate postnatal intake or absorption to match intrauterine mineral accretion rate
Risk factors
- <32 weeks’ gestation or <1500 g birth weight
- Male gender
- Delay in establishing enteral feeds/enteral feeds with low mineral content/bioavailability [unfortified expressed breast milk (EBM), term formula]
- PO4/Ca or vitamin D deficiency
- Prolonged parenteral nutrition (PN) (>2 weeks)
- Chronic drug use that increases mineral excretion (diuretics, steroids, sodium bicarbonate)
- Lack of mechanical stimulation e.g. sedation/paralysis
- Chronic lung disease
- Cholestatic jaundice
- Short gut syndrome (malabsorption of vitamin D and Ca)
Symptoms and signs
- ≤6 weeks – most babies are asymptomatic and normal on examination
- Usually presents aged 6–12 weeks
- Poor weight gain or faltering growth
- Respiratory difficulties: failure to extubate due to increased chest wall compliance
- Fractures with minor or no trauma; may manifest as pain on handling
- Craniotabes (softening of skull bones)
Later clinical consequences
- Marked dolicocephaly (long and narrow skull)
- Reduced linear growth
DIAGNOSIS
Serum biomarkers
- Low serum PO4 (<1.8 mmol/L) with elevated alkaline phosphatase (ALP) (>900 IU/L) is 100% sensitive and 70% specific for diagnosing low bone mineral density
- Low serum PO4 concentrations (<1.8 mmol/L) have 96% specificity but only 50% sensitivity. Routine PO4 supplementation in high risk babies could lead to secondary hyperparathyroidism, and thus worsen MBD
- Serum Ca levels may remain normal until late in the disease despite bone losses of Ca
- In suspected MBD with elevated ALP and low PO4, serum parathormone (PTH) measurement will help in establishing if there is underlying Ca or PO4 deficiency to provide correct supplementation
- Ca deficiency causes increased PTH to maintain normocalcaemia
- in PO4 deficiency there is no compensatory mechanism – PTH remains normal
Urinary biomarkers
- Urinary excretion of Ca >1.2 mmol/L and PO4 >0.4 mmol/L signifies slight surplus of supply and correlates with highest bone mineral accretion rate
- phosphaturia can occur due to aminoglycoside, indomethacin and steroid therapy
- calciuria can occur due to diuretics, steroids and theophylline
- Tubular reabsorption percent (TRP) of PO4 is also a guide to adequacy of PO4 supplementation. TRP of >95% indicates inadequate supplementation
- TRP (%TRP) = [1 − (urine PO4/urine creatinine) (plasma creatinine/plasma PO4)] x 100
Radiological
- Low bone density on X-rays (rachitic changes, cortical thinning, periosteal elevation) or fractures of long bones or ribs
- Dual-energy X-ray absorptiometry/qualitative ultrasound to assess bone mineral density
PREVENTION
- Optimal nutritional intake
- early PN with optimised Ca and PO4 content – Parenteral nutrition guideline
- early enteral feeds
- optimal ratio of enteral Ca:PO4 of 1.3:1–≤1.4:1 mmol-to-mmol basis should be targetted to avoid secondary hyperparathyroidism
- adequate Ca (3–5.0 mmol/kg/day) and PO4 (2.2–3.7 mmol/kg/day) intake by using fortified EBM or preterm formula. ≥140 mL/kg/day fortified EBM or preterm formula is needed to provide this
- daily intake of ≥400–700 units/kg/day vitamin D
- Ensure appropriate handling and position using deep boundaries to promote active bone loading
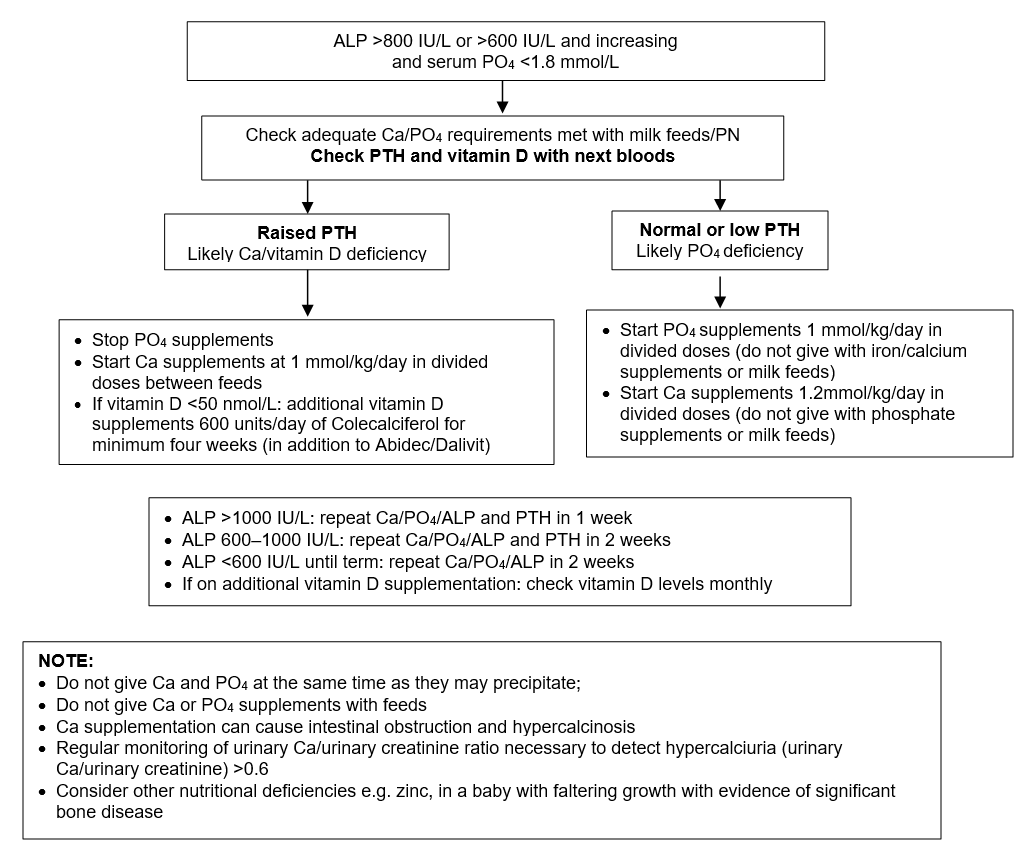
INVESTIGATION AND TREATMENT
For all high risk babies, after at least one week of full enteral feeds (≥140 mL/kg/day fortified EBM or preterm formula), measure serum Ca, PO4 and ALP levels from third week of life and follow this guidance:
MONITORING AND FOLLOW-UP
- Stop additional vitamin D when vitamin D and PTH are normal
- Adjust Ca dose based on serum Ca levels and stop only once PTH levels normalise
- Adjust PO4 dose based on serum PO4 levels, and ALP adjusting Ca dose to maintain ratios
- Continue treatment until biochemical indices are normal and radiographic evidence of healing, usually until term corrected gestation
Date updated: 2024-02-05