RECOGNITION AND ASSESSMENT
Definition
- Persistent patency of the ductus arteriosus (PDA) is a failure of functional ductal closure by 48 hr or anatomical closure by aged 3 weeks
Factors associated with delayed closure
- Prematurity (significant PDA affects approximately 30% of very-low-birth-weight babies)
- Lack of antenatal corticosteroid prophylaxis
- Surfactant-deficient lung disease
- Hypoxaemia
- Volume overload
Adverse effects of PDA
- Haemodynamic consequences of left-to-right shunt in preterm babies can prolong ventilatory support and are associated with mortality and morbidity [chronic lung disease, pulmonary haemorrhage, intraventricular haemorrhage, necrotising enterocolitis (NEC) and retinopathy of prematurity]
- Increased pulmonary blood flow (leading to increased work of breathing and respiratory deterioration)
- Reduced systemic blood flow (leading to acidosis and hypotension)
Symptoms and signs
- Can be absent even in the presence of a significant duct in first 7 days of life
- A significant left-to-right shunt is suggested by:
- bounding pulses and wide pulse pressure (i.e. >25 mmHg)
- hyperdynamic precordium (excessive movement of precordium)
- low-pitched systolic or continuous murmur over left upper sternal edge (absence of a murmur does not exclude significant PDA)
- signs of cardiac failure (tachypnoea, tachycardia, hepatomegaly, pulmonary oedema, generalised oedema etc.)
- poor perfusion (hypotension, poor capillary refill, mottled skin and persistent acidosis)
- increased or persistent ventilatory requirements
Differential diagnosis
- Other cardiac pathology (e.g. congenital heart disease, including duct-dependent lesions, arrhythmias or cardiomyopathy)
- Sepsis
INVESTIGATIONS
- SpO2 monitoring
- Chest X-ray (cardiomegaly? pulmonary plethora?)
- Echocardiography
- to detect duct-dependent cardiac lesions and other cardiac pathologies that are difficult to exclude clinically
- if considering treatment with prostaglandin inhibitor
- echocardiographic assessment of significant PDA includes:
- size of PDA (>1.5 mm)
- volume loading of left atrium (LA/aorta ratio >1.5)
- volume loading of left ventricle
- velocity and flow pattern of ductal flow
IMMEDIATE TREATMENT
General measures
- Optimise oxygenation by appropriate ventilatory management
- Use of a higher PEEP (i.e. ≥5 cm H2O) can help minimise effects of pulmonary oedema and risk of pulmonary haemorrhage
- Treat anaemia – maintain Hb ≥100 g/L with blood transfusion (consider concurrent dose of furosemide IV)
- Before starting medication, consider restricting fluid intake to 60–80% (e.g. from 150 mL/kg/day to 90–120 mL/kg/day)
- If fluid overload or pulmonary oedema, give 1 dose of furosemide IV in accordance with Neonatal Formulary
Specific measures
- Aim to convert haemodynamically significant PDA into insignificant PDA as complete duct closure may take weeks or months
Pharmacological treatment with prostaglandin inhibitor to initiate closure
Discuss with senior before starting or altering pharmacological treatment for PDA
- Ibuprofen IV is the drug of choice for this purpose – indometacin is not currently available in the UK
- if ibuprofen contraindicated discuss use of paracetamol with consultant (see below):
- be aware of the lack of data for long-term safety on the developing immature brain
- if ibuprofen contraindicated discuss use of paracetamol with consultant (see below):
- Pharmacological treatment is best used aged ≤2 weeks but can be effective ≤6 weeks
Indications for pharmacological treatment
- Babies born <34 weeks’ gestation with significant PDA – on clinical and/or echocardiographic assessment
- Includes ventilatory/CPAP dependent babies or PDA with haemodynamic effects (i.e. cardiac failure or poor perfusion)
- Monitor babies with non-significant PDA carefully and treat if becomes significant
IBUPROFEN
Contraindications
- Duct-dependent cardiac lesion
- Significant renal impairment: urine output <1 mL/kg/hr or creatinine >120 micromol/L
- Significant thrombocytopenia, i.e. platelet count <50 –109/L (course started or next dose given only after platelet transfusion)
- Suspected or definite NEC or gastrointestinal perforation
- Active phase of significant bleeding (gastrointestinal or severe intracranial) – treat coagulopathy before starting course (see Coagulopathy guideline)
Dose
- Calculate carefully and prescribe individually on single dose part of prescription chart so that contraindications checked before each dose
- Administer IV in accordance with Neonatal Formulary
Monitoring during treatment
- Check the following before each dose:
- creatinine (<120 micromol/L)
- urine output (>1 mL/kg/hr)
- platelet count (≥50 –109/L with platelet infusions if needed)
- If any parameter abnormal withhold dose until it normalises
PARACETAMOL
Contraindications
- Duct dependent cardiac lesion
Dose
- Dose and regimen as per local trust policy or formulary
- IV loading dose 20 mg/kg followed by IV maintenance dose of 10 mg/kg/dose 6-hrly. (This lower IV cumulative dose 40–50 mg/kg/day has been found to be effective and safe in RCTs
- Paracetamol 15 mg/kg/dose 6-hrly oral (total cumulative dose 60 mg/kg/day) has also been shown to be safe and effective in RCTs – consider this route if IV access difficult
- Repeat echo 3–5 days after commencing treatment
- Duration of treatment is 3 days but can be extended by a maximum of 3 more days if PDA remains significant (based on clinical or echo evaluation)
Monitoring during treatment
- Serum paracetamol trough levels before 3rd and 6th maintenance doses, and before every 3rd dose after any changes in frequency/dose
- therapeutic range 15–25 mg/L
- if levels >25 mg/L, reduce frequency/dose of paracetamol medication and recheck the pre-dose level before every 3rd dose after the change
- therapeutic range 15–25 mg/L
- LFTs before treatment, then daily for 6 days
- Echo day 3–5 of treatment
SUBSEQUENT MANAGEMENT (BOTH DRUGS)
- Aim to avoid concomitant nephrotoxic drugs e.g. gentamicin or vancomycin. Monitor levels or use an alternative drug
- Observe for signs of feed tolerance (feeds cautiously initiated or continued during treatment – briefly stopped during actual infusion)
- Monitor clinical signs of PDA and baby’s progress
- Echocardiography (if clinically indicated), repeated after 2–3 days of completion
- Fluid gradually liberalised after treatment based on:
- daily weight (weight gain suggests fluid retention)
- serum sodium (dilutional hyponatraemia common)
Persistence of recurrence of asymptomatic PDA
- Persistence of murmur does not necessarily indicate return of PDA
- Echocardiogram sometimes demonstrates physiological branch pulmonary stenosis
- If baby with asymptomatic murmur is making progress, plan echocardiography before discharge to decide follow-up
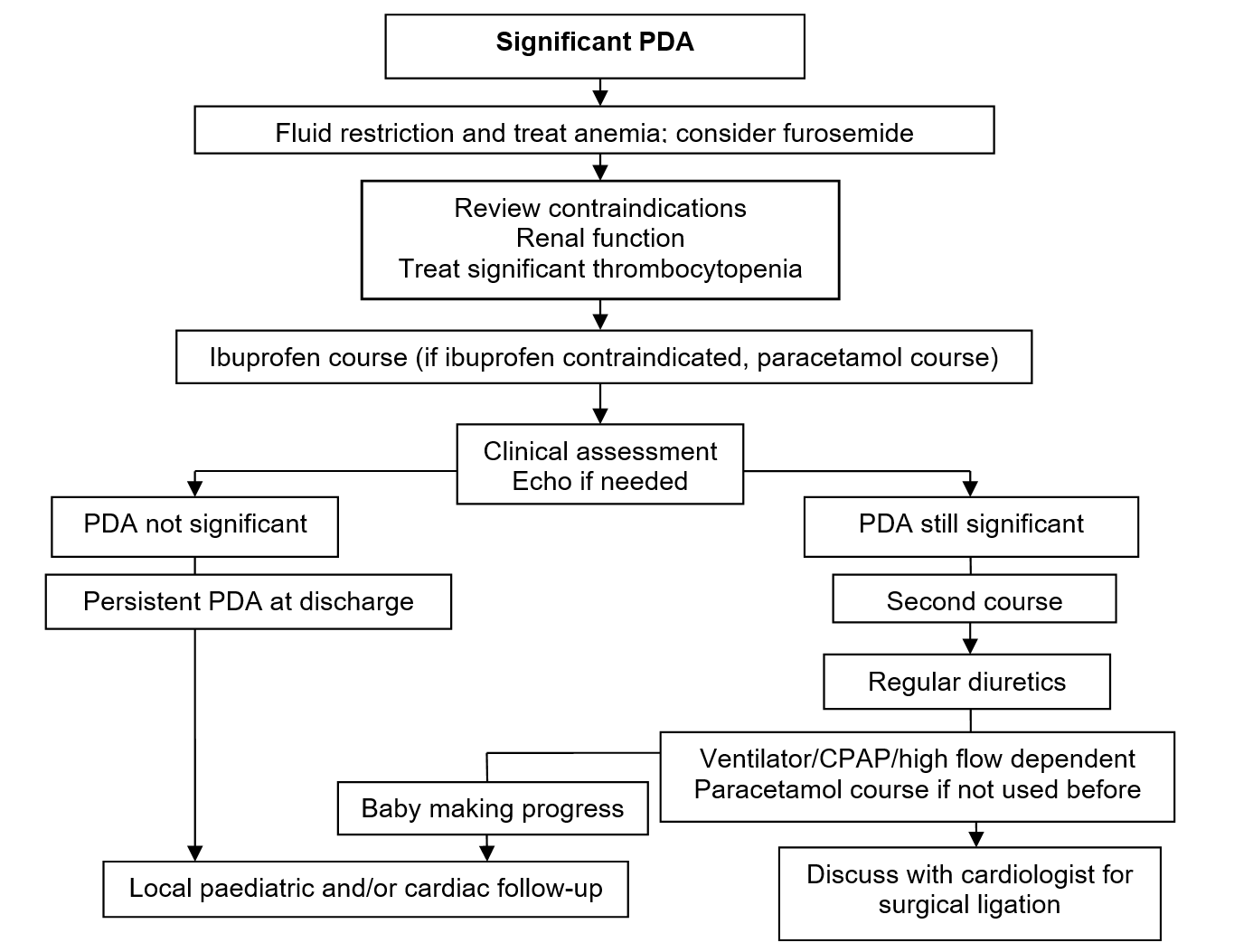
Persistent significant PDA and surgical referral
- If PDA significant after 48 hr of completion of first course of prostaglandin inhibitor, use second course of ibuprofen
- If PDA still significant but baby making progress (i.e. can be extubated or come off CPAP):
- commence regular diuretics (furosemide + amiloride/spronolactone) to help control haemodynamic effects/cardiac failure – in accordance with Neonatal Formulary
- monitor closely
- If PDA still significant and baby ventilatory or CPAP/high flow dependent, discuss with cardiac centre for surgical ligation when:
- prostaglandin inhibitor contraindicated
- if ibuprofen contraindicated, use paracetamol
- prostaglandin inhibitor not indicated (≥34 weeks with cardiac failure not controlled by diuretics)
- prostaglandin inhibitor ineffective (usually after giving second course). Paracetamol used as third course if not used before, while considering surgical ligation
- prostaglandin inhibitor contraindicated
- Discuss further cardiac assessment and surgical ligation of PDA with cardiologist at regional cardiac centre and transport team – follow local care pathway
- After surgical ligation, keep baby nil-by-mouth for 24 hr before gradually building up feeds (because of risk of NEC)
DISCHARGE POLICY FOR PERSISTENT PDA
- If PDA persistent clinically or echocardiographically at discharge or at 6 weeks follow-up, arrange further follow-up in cardiac clinic (locally or at cardiac centre depending on local practice)
- If PDA reviewed locally still persistent at aged 1 yr or if clinically significant during follow-up (cardiac failure or failure to thrive), refer to paediatric cardiologist at regional cardiac centre to consider closure (first option is usually catheter closure)
Medical treatment of persistent PDA <34 weeks' gestation
Date updated: 2024-01-10