- Check equipment daily, and before resuscitation
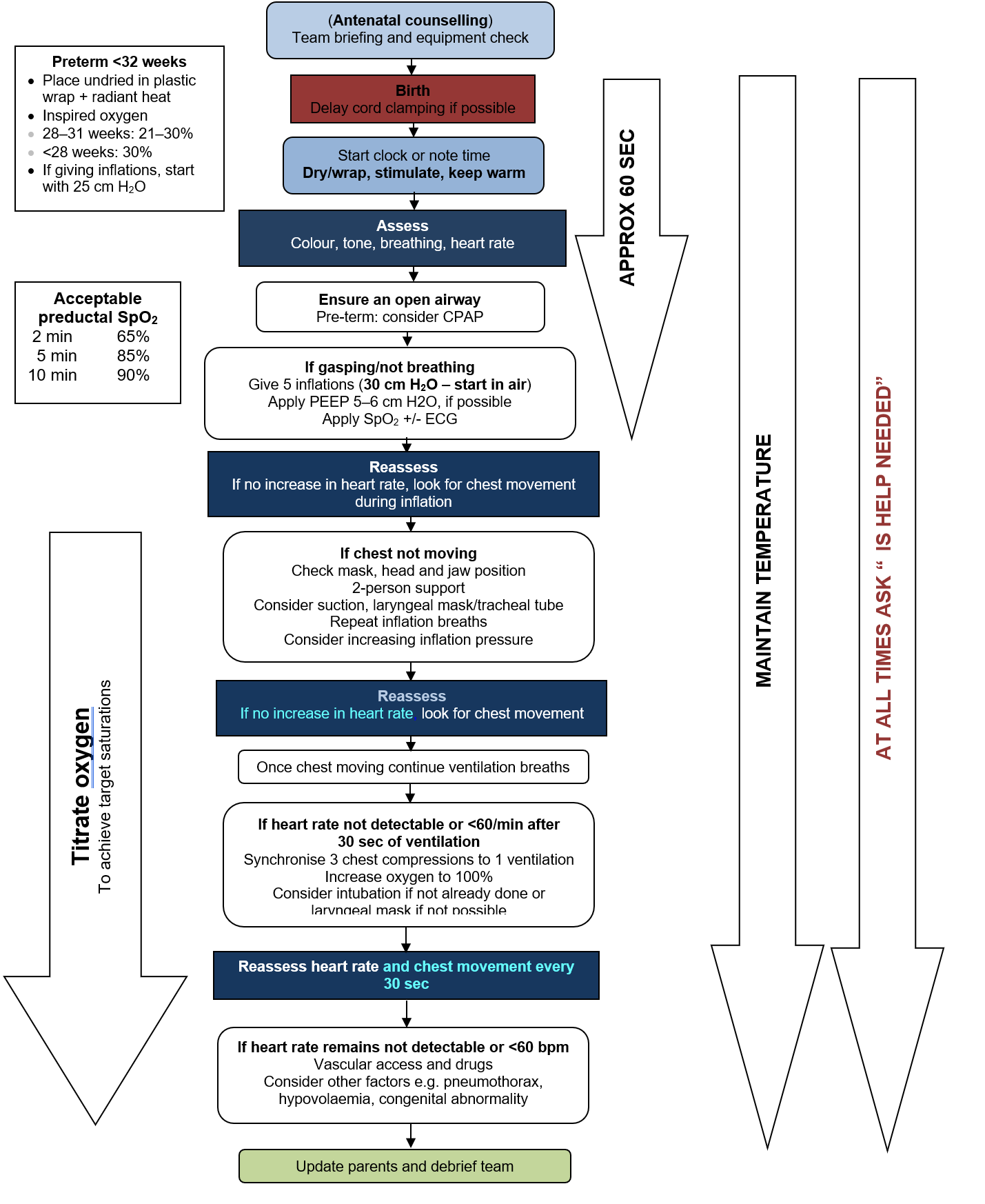
- Follow Resuscitation Council UK Guidelines https://www.resus.org.uk/library/2021-resuscitation-guidelines/newborn-resuscitation-and-support-transition-infants-birth
- Ensure delivery room is warm (23–25°C), windows closed and fans switched off
- Delivery room should be >25°C for babies ≤28 weeks gestation
CORD CLAMPING
- Uncompromised term and preterm babies: delay cord clamping (DCC) for ≥1 min from complete delivery of baby
- Stripping (milking) of the cord can be performed in babies ≥28 weeks’ gestation if DCC not feasible
- If immediate resuscitation required, clamp cord as soon as possible
DRY AND COVER
- ≥32 weeks’ gestation: dry baby, remove wet towels and cover baby with warm, dry towels
- <32 weeks’ gestation: do not dry body but place baby in plastic bag/sterile suit (Neohelp™ bag) feet first, and tuck in sides at the neck to fully enclose baby’s torso. Dry head only and put on hat
- Aim to maintain body temperature 36.5–37.5°C (unless decision taken to start therapeutic hypothermia)
- Preterm ≤32 weeks’ gestation may require additional interventions to maintain target temperature:
- warmed humidified respiratory gases
- thermal mattress alone
- increased room temperature (to 25°C) plus plastic wrapping of head and body, plus thermal mattress
ASSESS
- Assess colour, tone, breathing and heart rate
- Reassess heart rate, breathing and chest movement every 30 sec throughout resuscitation process
- If help required, request immediately
CHECK AIRWAY
- To open airway, place baby supine with head in ‛neutral position’
- If very floppy, give chin support or jaw thrust while maintaining the neutral position
IMMEDIATE TREATMENT
Airway
- Keep head in neutral position
- Use T-piece and soft round face mask, extending from nasal bridge to chin
- Give 5 inflation breaths, sustaining inflation pressure (Table 1) for 2–3 sec for each breath
- Give peak end expiratory pressure (PEEP) of 5 cm H2O
- Inflation breaths:
- term: start in air
- preterm
- ≥32 weeks: start in air
- 28–31 weeks: use low oxygen concentration (21–30%)
- preterm <28 weeks; use 30%
- Look for chest movement
Table 1: Inflation pressure (avoid using pressure higher than recommended)
| Term baby | 30 cm H2O |
| Preterm baby | 25 cm H2O |
No chest movement
Ask yourself:
- Is head in neutral position?
- Is a jaw thrust required?
- Do you need a second person to help with airway to perform 2-handed jaw thrust?
- Is there an obstruction and do you need to look with a laryngoscope and suck with a large-bore device?
- Consider intubation to secure airway if skilled, or placing a laryngeal mask airway (LMA) or i-gel under direct vision using laryngoscope in babies ≥34 weeks/>2 kg
- i-gels have been used in babies down to 1.5 kg
- Insertion of oropharyngeal airway or naso-pharyngeal airway if unable to secure airway by other means
- Is inflation time long enough?
- if no chest movement occurs after alternative airway procedures above have been tried (volume given is a function of time and pressure), a larger volume can be delivered if necessary by inflating for a longer time (3–4 sec) or gradually by increasing the peak inspiratory pressure (PIP)
- Attach saturation monitor to right hand – see Saturation monitoring for guidance on SpO2 targets
Endotracheal intubation
- Nasal continuous positive airway pressure (CPAP) rather than routine intubation may be used to provide initial respiratory support of all spontaneously breathing preterm babies with respiratory distress
Indications[/heading3
- Severe hypoxia (e.g. terminal apnoea or fresh stillbirth)
- Stabilisation of airway
- Congenital diaphragmatic hernia [see Congenital diaphragmatic hernia (CDH) guideline]
- to be electively intubated by most experienced person present
- NEVER give mask ventilation
If you cannot insert an ETT within 30 sec, revert to mask ventilation
Capnography can help to assess ETT placement (see Intubation guideline)
Breathing
- Most babies have a good heart rate after birth and establish breathing by 90 sec
- if not breathing adequately give 5 inflation breaths, preferably using air at pressures in Table 1
- Heart rate should rapidly increase as oxygenated blood reaches heart
Review assessment after inflation breaths
- Is there a rise in heart rate?
- Is there chest movement with the breaths you are giving?
- If no spontaneous breathing, provided the heart rate has increased and chest movement has been obtained, perform 30 sec of ventilation breaths, given at a rate of 30 breaths/min (1 sec inspiration)
Table 2: Outcome after 30 sec of ventilation breaths
| Heart rate | Breathing | Action |
| Increases | Not started breathing |
|
| <60 bpm | Obvious chest movement |
|
- Increase inspired oxygen concentration to 100%
Chest compression
- Use if heart rate approximately <60 bpm (do not try to count heart rate accurately as this will waste time)
Figure 1
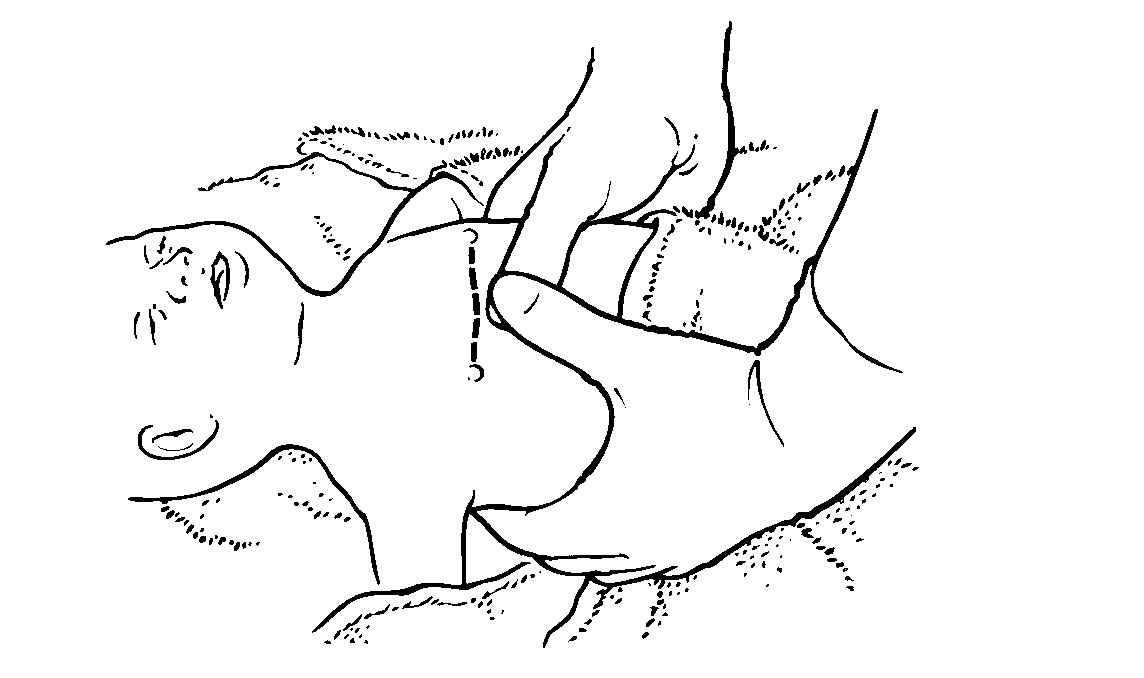
Figure2
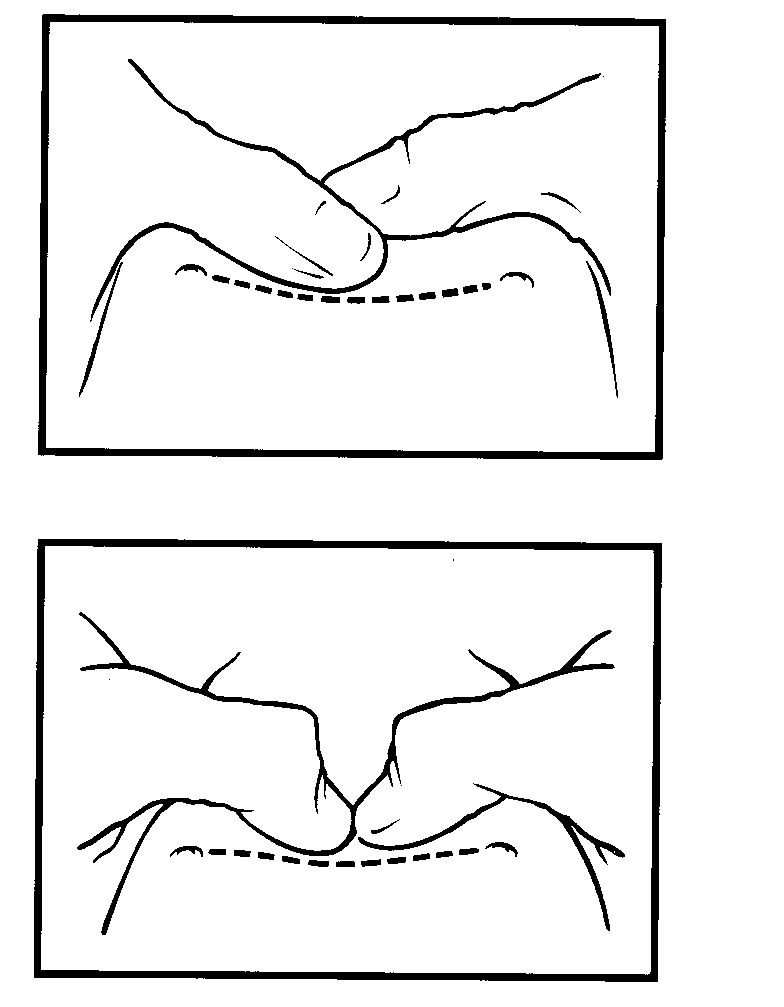
Pictures taken from NLS manual and Resuscitation Council (UK) and reproduced with their permission
Ideal hold (Figure 1/Figure 2)
- Circle chest with both hands so that thumbs can press on the sternum just below an imaginary line joining the nipples with fingers over baby’s spine
Alternative hold (less effective)
- Compress lower sternum with fingers while supporting baby’s back. The alternative hand position for cardiac compressions can be used when access to the umbilicus for umbilicus venous catheterisation is required, as hands around the chest may be awkward
Action
- Compress chest quickly and firmly to reduce the antero-posterior diameter of the chest by about one-third, followed by full re-expansion to allow ventricles to refill
- remember to relax grip on the chest during IPPV, and feel for chest movement during ventilation breaths, as it is easy to lose neutral position when cardiac compressions are started
Aim for 3:1 ratio of compressions to ventilations
and 90 compressions and 30 breaths (120 ‛events’) per min
Resuscitation drugs
- Always ask about drugs taken recently by, or given to mother
- Give drugs only if there is an undetectable or slow heartbeat despite effective lung inflation and effective chest compression
- Umbilical venous catheter (UVC) is the preferred route for urgent venous access
- Intraosseous (IO) access can be an alternative method of emergency access for drugs/fluids
- Recommence cardiac compressions and ventilation breaths ratio 3:1 after each drug administration and re-assess after 30 sec
- If no heart rate increase, progress onto next drug
Adrenaline 1:10,000
- 0.2 mL/kg (20 microgram/kg) 1:10,000 IV, repeated every 3–5 min
- Administration via ETT, use only when IV access not available; dose is 1 mL/kg (100 microgram/kg) 1:10,000
Sodium bicarbonate 4.2%
- 1–2 mmol/kg (2–4 mL/kg) IV (never give via ETT)
Glucose 10%
- 2.5 mL/kg IV slowly over 5 min
Sodium chloride 0.9%
- 10 mL/kg IV
Blood
- If there is evidence of fetal haemorrhage and hypovolaemia, consider giving O negative emergency blood
Naloxone
- Give only after ventilation by mask or ETT has been established with chest movement seen and heart beat >100 bpm
- If mother has been given pethidine within 2–4 hr of delivery, give naloxone IM:
- 100 microgram (0.25 mL) for small preterm babies
- 200 microgram (0.5 mL) for all other babies
WHEN TO STOP
- If no sign of life after 20 min, outlook is poor with few survivors, majority will have cerebral palsy and learning difficulties
ONGOING MANAGEMENT
Saturation monitoring
- Oxygen monitoring is activated when paediatrician/2nd pair of hands arrives. In the meantime, the person initiating resuscitation carries out all the usual steps in resuscitation
- Do not stop resuscitation for a saturation probe to be attached
- Attach saturation probe to the right hand and connect to the monitor once 5 inflation breaths have been given
- SpO2 should spontaneously improve as Table 3
Table 3
|
Time (min) |
Acceptable preductal SpO2 (%) |
| 2 | 65 |
| 5 | 85 |
| 10 | 90 |
Heart rate monitoring
- Best by listening with stethoscope
- Pulse oximetry
- ECG monitoring, if available, can give rapid accurate and continuous heart rate reading. However it does not indicate the presence of a cardiac output and should not be the sole means of monitoring
Air to oxygen
- Titrate the oxygen to saturation levels once SpO2 trace has been obtained
- If chest compressions required following chest movement with inflation breaths, increase oxygen to 100%
- If SpO2 above levels in Table 3 or >95% at 10 min of life, reduce oxygen
Meconium deliveries
- Do not attempt to suction nose and mouth whilst head is on perineum
- In non-vigorous babies born through meconium, immediate laryngoscopy with/without suction after delivery not recommended
- Only intubate if suspected tracheal obstruction, routine intubation is not necessary
Preterm deliveries
- Nasal CPAP rather than routine intubation may be used to provide initial respiratory support of all spontaneously breathing preterm babies with respiratory distress. Give PEEP at 5 cm H2O via mask ventilation with oxygen supplementation as appropriate on the resuscitaire and continue PEEP support during transfer to NICU
- If respiratory effort is poor at any point, or baby’s condition deteriorates, intubate and ventilate
DOCUMENTATION
- Make accurate written record of facts (not opinions) as soon as possible after the event
- This should be recorded on the BadgerNet system. In babies where resuscitation has been unsuccessful, a new baby episode of ‘labour ward death’ should be created and resuscitation documentation completed
- Record:
- when you were called, by whom and why
- condition of baby on arrival
- what you did and when you did it
- timing and detail of any response by baby – time of first HR, first HR >100, first gasp if any, and when spontaneous breathing resumed
- date and time of writing your entry
COMMUNICATION
- Inform parents what has happened (the facts)
NEWBORN LIFE SUPPORT ALGORITHM