Neonatal seizures are a manifestation of neurological dysfunction. Seizures occur in 1–3% of term newborn babies and in a greater proportion of preterm babies. They can be subtle, clonic, myoclonic or tonic
RECOGNITION AND ASSESSMENT
Physical signs
In addition to obvious convulsive movements, look for:
- Eyes: staring, blinking, horizontal deviation
- Oral: mouthing, chewing, sucking, tongue thrusting, lip smacking
- Limbs: boxing, cycling, pedalling
- Autonomic: apnoea, tachycardia, unstable blood pressure
- Focal (1 extremity) or multifocal (several body parts)
- Perform a detailed physical examination and neurological assessment
Differential diagnosis
- Jitteriness: tremulous, jerky, stimulus-provoked and ceasing with passive flexion
- Benign sleep myoclonus: focal or generalised, myoclonic limb jerks that do not involve face, occurring when baby is going to or waking up from sleep; EEG normal; resolves by aged 4–6 months
- Differentiation between jitteriness and seizures:
Table 1
| Sign | Jitteriness | Seizure |
| Stimulus provoked | Yes | No |
| Predominant movement | Rapid, oscillatory, tremor | Clonic, tonic |
| Movements cease when limb is held | Yes | No |
| Conscious state | Awake or asleep | Altered |
| Eye deviation | No | Yes |
Investigations
First line
- Blood glucose
- Serum electrolytes including calcium, magnesium
- FBC and coagulation (if stroke suspected, thrombophilia screen)
- Blood gases
- Blood culture
- CRP
- LFT
- Serum ammonia, amino acids
- Urine toxicology, amino acids, organic acids
- Lumbar puncture – CSF microscopy and culture (bacterial and viral PCR for herpes simplex including enterovirus)
- discuss CSF sample for further metabolic testing [e.g. glycine, lactate etc. (as guided by metabolic testing)] with consultant
- Cranial ultrasound scan (to exclude intracranial haemorrhage)
EEG (to identify electrographic seizures and to monitor response to therapy). Consider cerebral function monitor (CFM–aEEG)
Second line
- Congenital infection screen (TORCH screen)
- MRI scan
- Screen for maternal substance abuse
- Serum acylcarnitine, biotinidase, VLCFA, uric acid, sulphocysteine, total and free homocysteine
- Trial of pyridoxine treatment, preferably during EEG monitoring, may be diagnostic as well as therapeutic
- If further advice required, contact metabolic team
TREATMENT
- Ensure ABC
- Treat underlying cause (hypoglycaemia, electrolyte abnormalities, infection)
- hypoglycaemia: give glucose 10% 2.5–5 mL/kg IV bolus, followed by maintenance infusion. Wherever possible, obtain ‘hypoglycaemia screen’ (see Hypoglycaemia guideline) before administration of glucose bolus
- hypocalcaemia (total Ca <1.7 mmol/L or ionised Ca <0.64 mmol/L): give calcium gluconate 10% 0.5 mL/kg IV over 5–10 min with ECG monitoring (risk of tissue damage if extravasation) (see Hypoglycaemia guideline)
- hypomagnesaemia (<1 mmol/L): give magnesium sulphate 100 mg/kg IV or deep IM (also use for refractory hypocalcaemic seizure)
- Pyridoxine (50–100 mg IV) can be given to babies unresponsive to conventional anticonvulsants or seek neurologist opinion
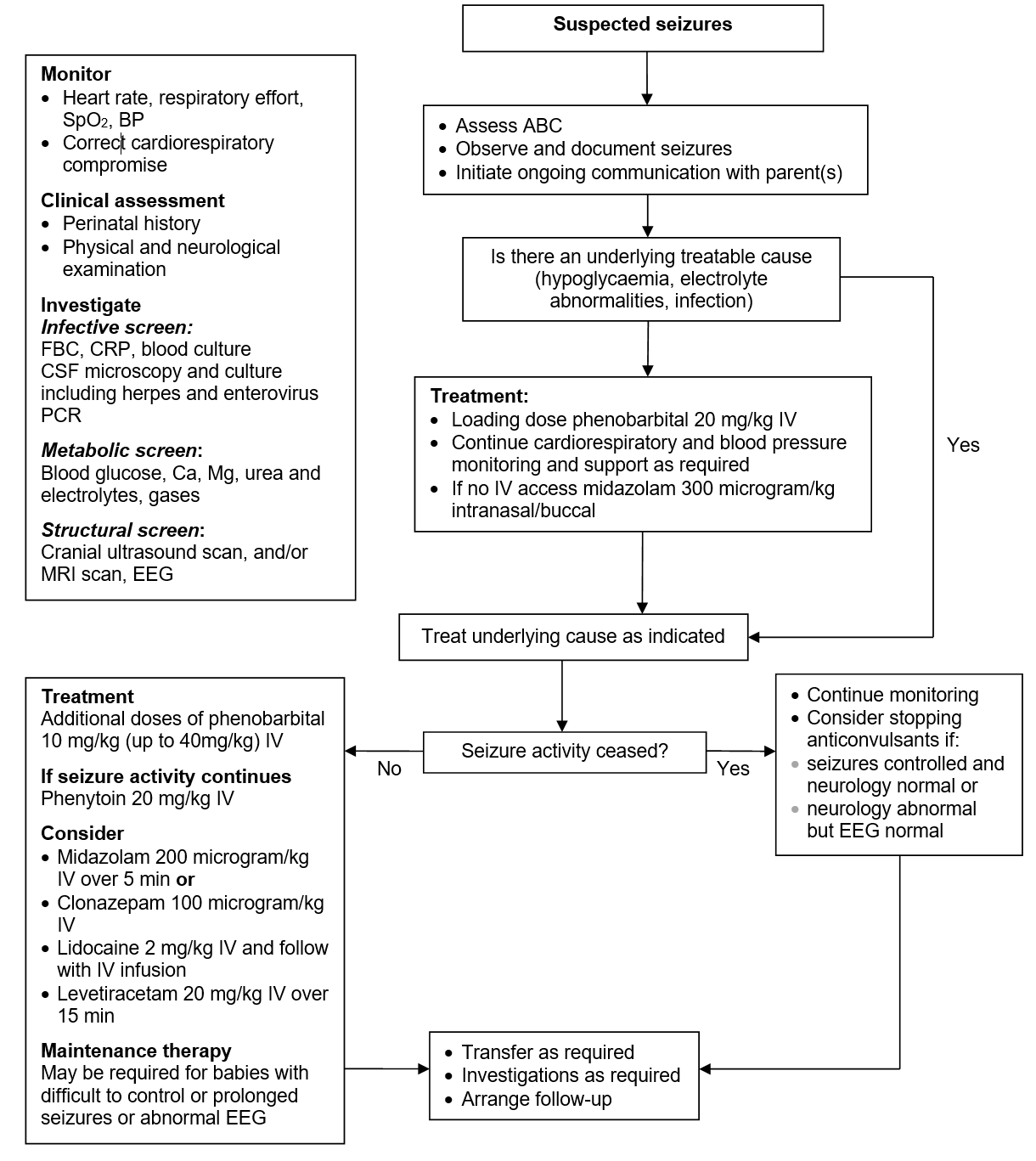
Initiation of anticonvulsants (for immediate management follow flowchart)
- Start anticonvulsant drugs when:
- prolonged: >2–3 min
- frequent: >2–3/hr
- associated with cardiorespiratory compromise (frequent apnoeas and bradycardia requiring intervention)
Management Flowchart
Administration
- IV to achieve rapid onset of action and predictable blood levels
- To maximum dosage before introducing a second drug
- If no IV access and glucose and electrolyte abnormalities excluded, consideration can be given to buccal/intranasal midazolam
Maintenance and duration of treatment
- Keep duration of treatment as short as possible. This will depend on diagnosis and likelihood of recurrence
- May not require maintenance therapy after loading dose
- If maintenance therapy is required:
- monitor serum levels
- develop emergency seizure management plan, including, if required, a plan for buccal/intranasal midazolam
Stopping treatment
- Consider:
- seizures have ceased and neurological examination is normal or
- abnormal neurological examination with normal EEG
Anticonvulsant drug therapy schedule
| Drug | Loading dose | Maintenance dose |
| Phenobarbital |
|
2.5–5 mg/kg IV or oral once daily beginning 12–24 hr after loading dose |
| Phenytoin |
|
|
| Midazolam (if no response to above drugs) |
|
|
| Clonazepam (if midazolam not available) |
|
|
| Lidocaine (if above medications ineffective) |
|
|
| Levetiracetam (if not responding in any order) |
|
|
DISCHARGE AND FOLLOW-UP
Discharge
- Ensure parents are provided with appropriate discharge documentation
- seizure emergency management plan
- copy of discharge summary, including: types of seizures, medications/anticonvulsants administered
Follow-up
- Follow-up will depend on cause of seizures and response to treatment
- Consider: specialist follow-up for babies discharged on anticonvulsant drugs
Further information for parents www.bcmj.org/sites/default/files/HN_Seizures-newborns.pdf
Date updated: 2024-01-15