See also Tuberculosis (investigation and management following exposure in pregnancy) guideline
INDICATIONS
- All babies (aged ≤12 months) with a parent or grandparent who was born in a country where the annual incidence of TB is ≥40/100,000
- All babies (aged ≤12 months) living in areas of the UK where the annual incidence of TB is ≥40/100,000
- PHE TB Official Statistics 2020 (publishing.service.gov.uk)
BCG vaccine to be given to eligible baby
- Once aged 28 days
- On receipt of screen negative severe combined immune deficiency (SCID) result (or ‘SCID not offered’ result)
Countries with incidence of TB ≥40/100,000
| Afghanistan | Ecuador | Korea DPR | Niger | Tajikistan |
| Algeria | El Salvador | Korea (Rep. of) | Nigeria | Tanzania |
| Angola | Equatorial Guinea | Kyrgyzstan | Niue | Thailand |
| Azerbaijan | Eritrea | Lao PDR | Northern Mariana Islands | Timor-Leste |
| Bangladesh | Eswatini | Lesotho | Pakistan | Turkmenistan |
| Benin | Ethiopia | Liberia | Palau | Tuvalu |
| Bhutan | Fiji | Libya | Panama | Uganda |
| Bolivia | Gabon | Lithuania | Papua New Guinea | Ukraine |
| Botswana | Gambia | Madagascar | Paraguay | Uzbekistan |
| Brazil | Georgia | Malawi | Peru | Vanuatu |
| Brunei | Ghana | Malaysia | Philippines | Venezuela |
| Burkina Faso | Greenland | Mali | Romania | Vietnam |
| Burundi | Guam | Marshall Islands | Russia | Yemen |
| Cambodia | Guinea | Mauritania | Rwanda | Zambia |
| Cameroon | Guinea-Bissau | Micronesia | Sao Tome and Principe | Zimbabwe |
| Cape Verde | Guyana | Moldova | Senegal | |
| Central African Republic | Haiti | Mongolia | Sierra Leone | |
| Chad | Hong Kong | Morocco | Singapore | |
| China | India | Mozambique | Solomon Islands | |
| Congo | Indonesia | Myanmar | Somalia | |
| Congo DR | Iraq | Namibia | South Africa | |
| Côte d'Ivoire | Kazakhstan | Nauru | South Sudan | |
| Djibouti | Kenya | Nepal | Sri Lanka | |
| Dominican Republic | Kiribati | Nicaragua | Sudan |
https://www.gov.uk/government/publications/tuberculosis-tb-by-country-rates-per-100000-people
Tuberculin testing not necessary aged <6 yr unless baby has been in recent contact with TB or has resided in high-incidence country for >3 months
CONTRAINDICATIONS
- SCID screen positive or screen performed and result pending
- Temperature >38°C or acutely unwell
- Severe eczema (give at suitable lesion-free site)
- Baby in household where an active TB case suspected or confirmed, see Tuberculosis (investigation and management following exposure in pregnancy) guideline
- Immunodeficient or on high-dose corticosteroids
- defer BCG until 3 months after stopping corticosteroids if given prednisolone 1 mg/kg/day for >2 weeks, 2 mg/kg/day for 1 week, (or equivalent doses of another corticosteroid, e.g. dexamethasone 150 micrograms = prednisolone 1 mg)
- Maternal immunosuppressive treatment during pregnancy or breastfeeding
- biologicals e.g. anti-TNFα, postpone BCG until aged 6 months
- immune-modulation therapy for treatment of COVID in pregnancy e.g. tocilizumab and sarilumab, postpone BCG until aged 6 months
- HIV positive, living in UK
- if mother HIV positive and high risk of HIV transmission [see Human immunodeficiency virus (HIV) guideline] and exclusively formula feeding, give vaccine only after baby is confirmed HIV uninfected at aged 12–14 weeks
- if mother HIV positive and very low risk or low risk of HIV transmission [see Human immunodeficiency virus (HIV) guideline] BCG can be given to baby when indicated
- if high risk of TB exposure and maternal HIV viral load <50 copies/mL after 36 weeks’ gestation, BCG can be given at birth
- encourage maternal HIV testing but do not withhold BCG if mother declines testing unless mother from sub-Saharan Africa, in which case refer to HIV team for counselling about testing
SPECIAL CASES
- No need to delay routine vaccinations
- BCG can be given simultaneously with other vaccines [including rotavirus vaccine oral or palivizumab (Synagis®) (IM but not in same arm)]
- no further immunisation should be given in arm used for BCG immunisation for ≥3 months due to risk of regional lymphadenitis
- if not given at same time, leave 4 weeks before giving other injectable live vaccines
PROCEDURE
- Dose: 0.05 mL (Note: vial contains 20 doses)
- Only to be given by health professional trained in giving BCG vaccine
Consent
- Midwife to record at booking if risk factor present
- Postnatal check for risk factor
- Ensure baby within inclusion group
- Give mother information on vaccine
- Give appropriate language leaflet TB, BCG vaccine and your baby, available from https://www.gov.uk/government/publications/tb-bcg-and-your-baby-leaflet order line: 0300 123 1002
- Department of Health guidelines state written consent is not required but follow local practice
Injection
Only staff trained to give intradermal injections to give BCG
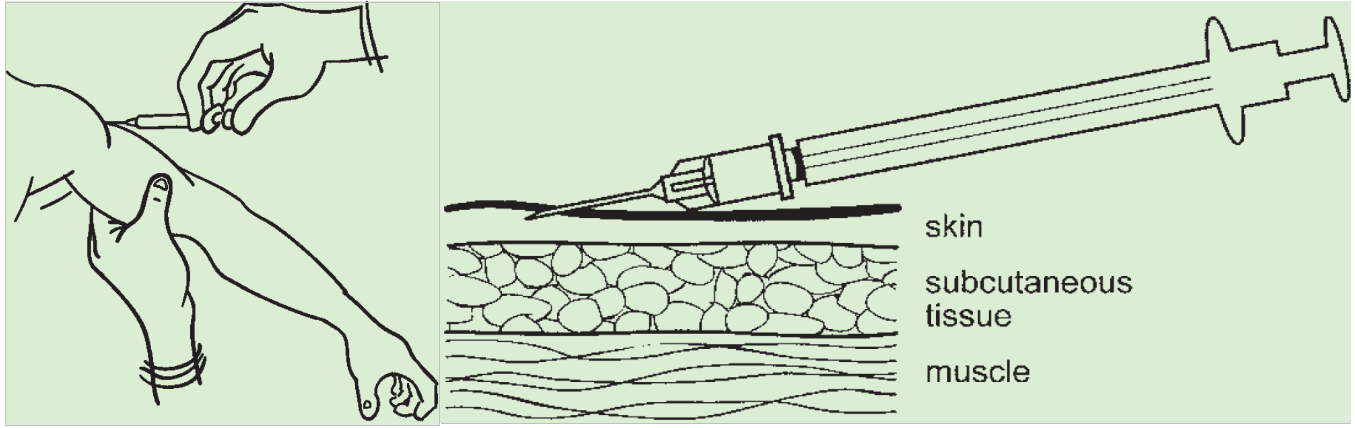
- Hold arm at 45° to body
- At insertion of deltoid muscle near middle of left upper arm
- If skin is clean, no further cleaning is necessary
- If skin is visibly dirty, clean with soap and water
- Stretch skin between thumb and forefinger
- Introduce needle bevel upwards approximately 3 mm into superficial layers of dermis almost parallel to skin
- If considerable resistance not felt, remove needle and reinsert before giving more vaccine
- Correctly given intradermal injection results a tense blanched bleb
DOCUMENTATION
- Enter on BCG page in online Child Health Record or in Red Book and tear out yellow copy for Child Health
SEQUELAE
- Scar
- within 2–6 weeks a small papule will appear
- sometimes this ulcerates and can ooze
- site need not be protected from water
- do not cover with an impervious dressing
- can take several months to heal
- occasionally persists as keloid (particularly if given superior to insertion of deltoid)
- Adenitis:
- a minor degree of adenitis can occur in the weeks following BCG
- no treatment indicated
- Rare sequelae:
- local abscess
- chronic suppurative lymphadenopathy
- disseminated disease, if immunocompromised
- osteitis, refer to infectious diseases specialist
Refer to paediatric TB team if
- Severe local reactions
- abscesses or drainage at the injection site or
- regional suppurative lymphadenitis with draining sinuses
Refer disseminated BCG infection to paediatric TB specialist
Date updated: 2024-02-05