DEFINITION
- There is no established definition of hyperglycaemia. However, treat if:
- 2 blood sugars ≥14 on 2 occasions measured ≥2 hr apart or
- blood sugars ≥12 on 2 occasions measured ≥2 hr apart with evidence of significant glycosuria (2+ on urine dipstick)
Do not take sample from an infusion line that has glucose running through it
CLINICAL FEATURES
- Osmotic diuresis leading to dehydration
- Poor weight gain
Risk factors
- Immaturity of pancreatic function (e.g. extremely premature infants and small-for-gestational-age)
- Insulin resistance
- Glucose overload (e.g. equipment failure, administrator error)
- Stress (e.g. infection, pain)
- Side effects of a medication (e.g. glucocorticoid treatment)
MONITORING
- Most blood gas machines provide glucose measurements
- Check blood glucose at least 6–8 hrly in:
- unstable or acutely ill babies [respiratory distress syndrome, septicaemia, necrotising enterocolitis (NEC)]
- Check blood glucose at least once a day in stable babies:
- <32 weeks’ gestation for first week
- receiving parenteral nutrition (PN)
- with severe unexpected dehydration or metabolic acidosis
- with poor weight gain while receiving >120 kcal/kg/day
Babies treated with corticosteroids
- Check urine for glycosuria daily
- Check blood glucose if ≥2+ glucose in urine
TREATMENT
- If possible, discontinue or decrease medications that worsen hyperglycaemia
- Lipid component of PN may contribute to worsening hyperglycaemia. If on PN discuss stopping lipid with consultant/pharmacist
Suspected infection/NEC
- Hyperglycaemia in baby with previously stable blood glucose may be an early indicator of infection or NEC
- Assess baby clinically
- After taking appropriate cultures, treat empirically
Fluids
- If blood glucose ≥12 mmol/L, check urine for glycosuria (of ≥2+) and assess clinical hydration and fluid input/output. Check for fluid administration errors
- Calculate amount of glucose baby is receiving (as mg/kg/min) using the formula:
| Glucose infusion rate (mg/kg/min) | = | % glucose x fluid rate (mL/kg/day) 144 |
- If glucose delivery rate >10 mg/kg/min, decrease glucose in decrements to
6–10 mg/kg/min. If on PN, 8–10 mg/kg/min is acceptable - If glycosuria and hyperglycaemia >12 mmol/L persists despite an appropriate glucose infusion rate, consider treating with insulin
Insulin
- Commence insulin therapy at 0.05 units/kg/hr and titrate according to response – see Administration of Actrapid® insulin (soluble insulin)
- Check blood glucose 1 hr from starting and hourly until target reached
- Increase the insulin by increments of 0.05–0.1 units/kg/hr. Target blood glucose while on insulin is 6–8 mmol/L
- Once blood glucose stable, continue to monitor blood glucose 4-hrly
- When a baby is on insulin it is very important to prevent hypoglycaemia – see below
Preventing hypoglycaemia
|
Blood glucose |
Insulin infusion rate |
| >8 |
|
| 6–8 |
|
| >4–<6 |
|
| ≤4 |
|
- Recheck blood glucose 1 hr after reducing dose, then 1–2 hrly until stable, then 4-hrly when stable
- If unable to wean off insulin after 1 week, transient neonatal diabetes is possible; consult paediatric endocrinologist
- Early introduction of PN and early trophic enteral feeding will help reduce incidence of hyperglycaemia requiring insulin
ADMINISTRATION OF ACTRAPID® INSULIN (SOLUBLE INSULIN)
- Follow instructions in Neonatal Formulary for making up insulin infusion
- Administer Actrapid® insulin infusion via a central line or dedicated peripheral cannula
- Before starting infusion, prime all IV connecting and extension sets and T-connectors with insulin infusion fluid. Check manufacturer’s guide on lumen capacity for priming volumes (insulin can adhere to the plastic of the syringe)
Summary of neonatal hyperglycaemia management
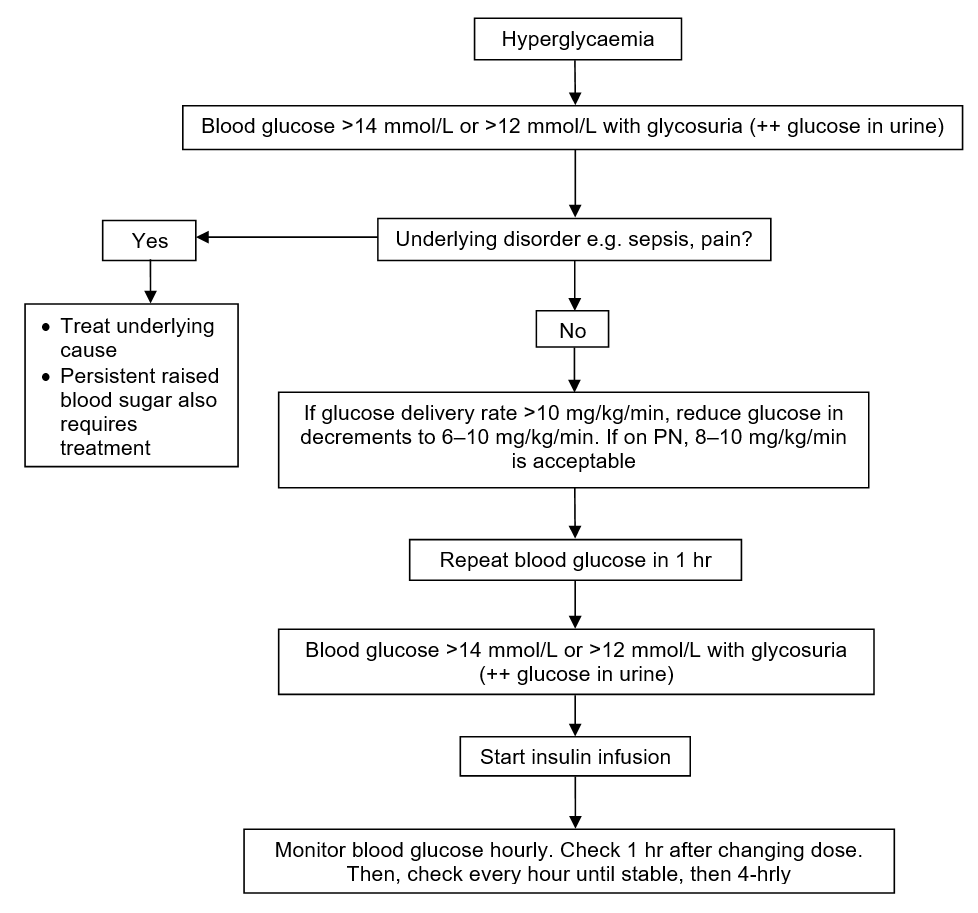
Avoid iatrogenic hypoglycaemia by careful, regular blood glucose monitoring
Date updated: 2024-02-05