RECOGNITION AND ASSESSMENT
- Term or preterm babies birth weight ≥1500 g: total serum calcium <2 mmol/L or ionised fraction <1.1 mmo/L
- Preterm baby, birth weight <1500 g: total serum calcium <1.75 mmol/L or ionised fraction <1 mmol/L
SYMPTOMS AND SIGNS
- Early onset occurs in first 2–3 days of life and is usually asymptomatic
- Late onset develops after first 2–3 days of life and typically occurs at the end of the first week
- Most babies are asymptomatic and identified on screening
- Characteristic sign is increased neuromuscular irritability including:
- jitteriness and irritability
- generalised/focal seizures
- non-specific symptoms e.g.:
- poor feeding
- lethargy
- apnoea
- prolonged QTc on ECG
- rare presentations:
- stridor
- bronchospasm
- pylorospasm
CAUSES
- Early onset:
- prematurity
- intrauterine growth restriction
- babies of diabetic mother
- hypoxic ischaemic encephalopathy
- hypomagnesaemia
- hypoparathyroidism
- syndromes e.g. DiGeorge syndrome
- maternal hyperparathyroidism
- Late onset:
- high phosphate load – cow’s milk, renal failure
- hypomagnesaemia
- parenteral nutrition
- exchange transfusion
- alkalosis
- maternal hypercalcemia
- maternal vitamin D deficiency
- transient hypoparathyroidism
- syndromes and genetic mutations e.g. DiGeorge and Kenny-Caffey syndromes
INVESTIGATIONS
- Serum calcium
- only monitor if risk factors, most babies with hypocalcaemia are asymptomatic
- well preterm baby with birth weight >1500 g and well term babies of diabetic mothers receiving milk feedings on day 1 of life do not need testing routinely
- ionised calcium preferred
- if using total calcium, measure albumin and correct for hypoalbuminemia
- Phosphate
- Magnesium
- Persistent hypocalcaemia or severe hypocalcaemia despite adequate calcium therapy:
- 25-hydroxyvitamin D level
- renal function tests
- liver function test
- alkaline phosphatase
- parathyroid hormone level
- urinary calcium:creatinine ratio
- ECG for prolonged QTc interval
- if pseudohyperparathyroidism suspected, X-ray hand
- chest X-ray for thymic shadow
- if hypoparathyroidism suspected, renal ultrasound
- if DiGeorge syndrome suspected, echocardiography
- genetic test for gene mutations or suspected syndrome e.g. DiGeorge syndrome
MANAGEMENT
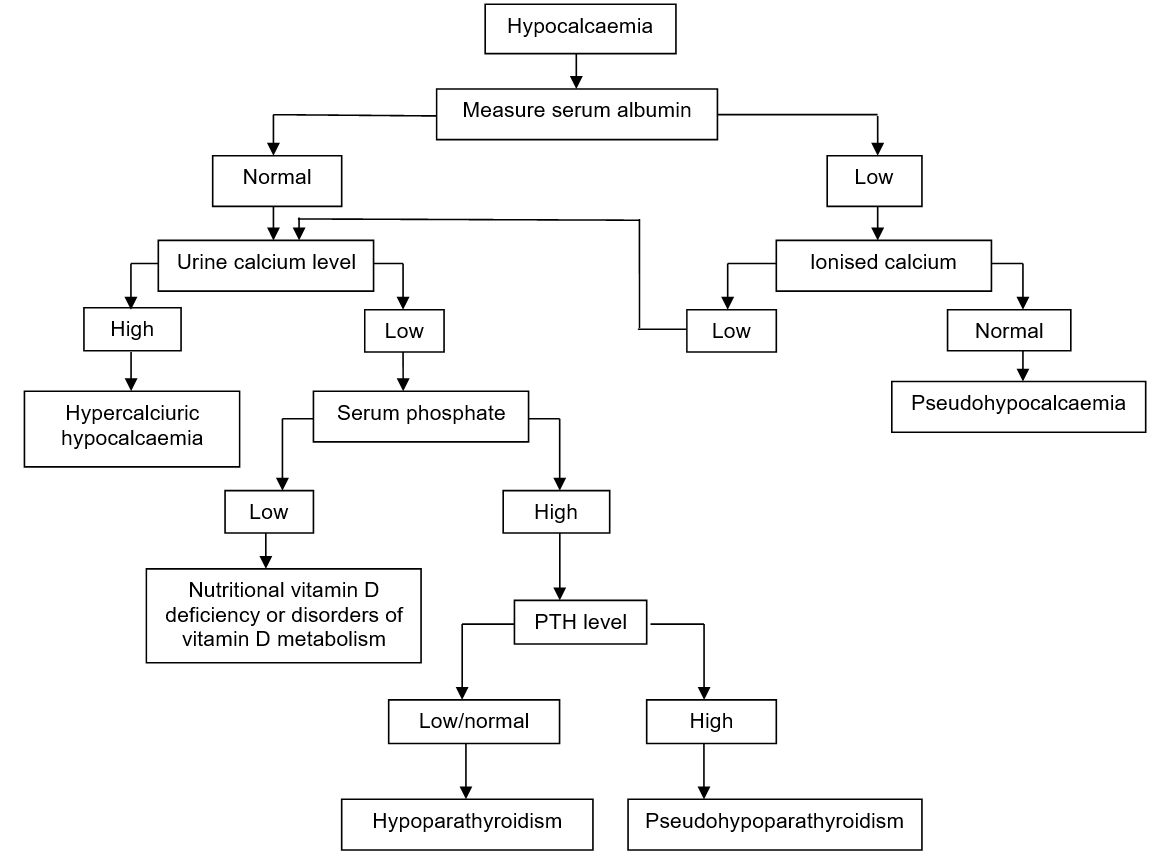
See Flowchart: Diagnostic approach to neonatal hypocalcaemia
Asymptomatic babies
- Most babies with early onset hypocalcaemia recover with nutritional support; so early feeding provides adequate calcium
- Babies requiring IV fluid: add calcium gluconate 10% 0.46 mmol/kg/day (= 2 mL/kg/day) to IV fluid and give as continuous infusion
- baby tolerating oral feeds: give 0.25 mmol/kg oral 6-hrly
Symptomatic hypocalcaemia
- If seizures, prolonged QT interval, apnoea, unstable, hypotension or poor feeding give IV calcium gluconate 10% 0.11 mmol/kg (= 0.5 mL/kg) over 5–10 min followed by maintenance
- dilute with sodium chloride 0.9% or glucose 5% 4 mL to each 1 mL calcium gluconate 10% to give a concentration of 45 micromol/mL. Can be given undiluted via central line in an emergency
- doses up to 0.46 mmol/kg (= 2 mL/kg calcium gluconate 10%) have been used
- maximum rate of administration 22 micromol/kg/hr
- Stable baby or following acute treatment
- oral calcium dose 0.25 mmol/kg 6-hrly
- if enteral feeds not tolerated add calcium gluconate 10% 0.5 mmol/kg/day to IV fluid as above
- If symptomatic hypocalcaemia: hypomagnesaemia – magnesium sulphate 100 mg/kg IV/ deep IM 12-hrly for 2–3 doses
- Vitamin D deficiency give 1000–2000 units daily and adjust dose according to response
- Hyperphosphataemia
- high calcium, low phosphate diet
- human milk is preferable, if not available, use formula with low phosphate 60/40 and oral calcium
IV calcium precautions and considerations
- Extravasation can cause skin and subcutaneous tissue necrosis (see Extravasation guideline). Monitor IV site closely
- Continuous infusion preferred to bolus, but use bolus for initial management in symptomatic hypocalcaemia
- Bolus IV calcium can cause dysrhythmias – administer slowly over 5–10 min with cardiac monitoring
- Calcium can be given via UVC provided catheter tip is in vena cava
- inadvertent administration into portal vein can cause hepatic necrosis
- Do not mix calcium solutions with those containing phosphorus or bicarbonate as this can cause precipitation
SUBSEQUENT MANAGEMENT
- Monitor bone profile and phosphate levels according to clinical need
- If calcium normal after 48 hr treatment, halve maintenance dose
- If calcium fails to normalise investigate for underlying cause
- For extreme preterm babies with late onset hypocalcaemia [see Metabolic bone disease (MBD) guideline]
- Hyperphosphataemia – calcium and phosphate normalise in 3–5 days. Stop calcium after 1 week and switch to normal formula in 2–4 weeks
Flowchart: Diagnostic approach to neonatal hypocalcaemia
Date updated: 2024-01-11