DEFINITION
- Cholestasis: conjugated bilirubin ≥25 micromol/L and/or ≥20% of total bilirubin
- Acute liver failure with raised transaminase and coagulopathy unresponsive to vitamin K
Discuss all babies with liver dysfunction at term urgently with liver unit team
CAUSES
- Not all liver dysfunction in preterm babies is caused by parenteral nutrition. Extra-hepatic biliary atresia does occur and must be diagnosed and managed in a timely fashion
| Biliary tract disorders | Neonatal hepatitis | Metabolic |
|
Isolated
|
|
| Infection | Endocrine | Toxins/injury |
|
|
|
SYMPTOMS AND SIGNS
- Pale or acholic stools
- Dark urine
- Prolonged jaundice (defined as visible jaundice at day 14 in term and day 21 in preterm babies)
- Bleeding, including intraventricular haemorrhage from vitamin K deficiency
- Green jaundice on any day of life
- Acute collapse with liver failure
- Hypoglycaemia
INVESTIGATIONS
Aim to diagnose causes of liver dysfunction that will benefit from early diagnosis while avoiding unnecessary transfer and investigation of small sick babies
First line investigations
- Complete the following as soon as possible:
- FBC and film
- coagulation screen
- blood gas – glucose and lactate
- transaminases, including ALT, AST, bilirubin (total and conjugated), albumin, gamma GT, and alkaline phosphatase, LDH, AFP, ferritin
- albumin
- galactosaemia and tyrosinaemia screen
- alpha-1 antitrypsin concentration and phenotype
- serum cortisol, T4 and TSH
- stool in opaque pot for consultant review
- urine for MC&S
- abdominal ultrasound scan, after 4 hr fast if possible, to include liver and gallbladder examination
- if clinical suspicion high toxoplasma serology, CMV IgM or urine PCR for CMV, syphilis serology, viral culture from swabs of any vesicles for herpes simplex, hepatitis E serology
- if metabolic disorder suspected, plasma lactate, plasma and urine amino acids, and urine organic acids, ammonia
- discuss with biochemistry before sampling (transport may need to be arranged)
As they become available, discuss results of liver function, coagulation, stool colour, weight gain and abdominal ultrasound with liver unit team
FURTHER INVESTIGATIONS
- Follow advice of liver team
- Standard aggressive protocol used to investigate term babies is inappropriate in preterm babies due to:
- insufficient blood volume for blanket testing
- poor temperature control when attending for isotope scans
- limited size increases risk of liver biopsy
- Transfer to specialist centre often not possible owing to need for ongoing respiratory support and neonatal nursing care
- Preterm babies with diagnoses requiring surgery (e.g. Kasai procedure for biliary atresia) need to be around 2 kg before surgery performed but liver team should be informed in advance of baby reaching this weight
- Early isotope scanning not widely available and of limited value, many babies can be investigated without this procedure – follow advice of liver team
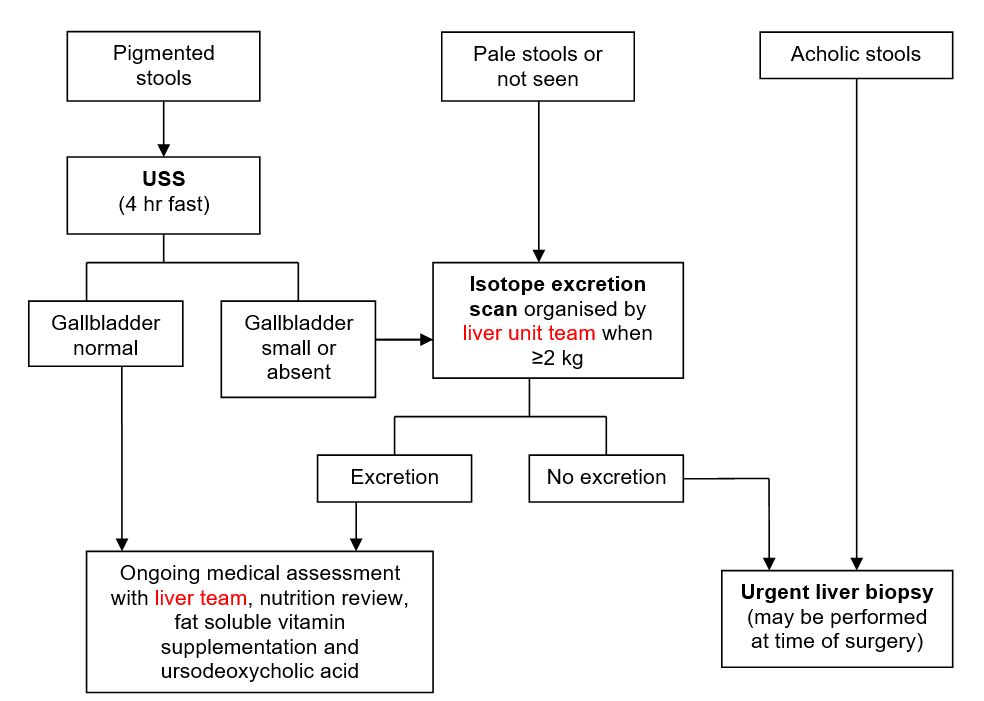
- Assessment of stool colour can determine which babies with cholestasis require urgent further investigation, as shown below:
Investigations for ongoing liver dysfunction
- If indicated by results of first line investigations or progressive dysfunction and on advice of liver team:
- ophthalmic review (other than for retinopathy of prematurity)
- micro-array for dysmorphism
- karyotype
- very long chain fatty acids for neurological abnormality
- urinary bile salts
- other congenital infections screen
- isotope scan, liver biopsy or bone marrow aspirate
MANAGEMENT OF CHOLESTASIS
- Surgical correction, if appropriate (e.g. Kasai, choledochal cyst), usually when around 2 kg, discuss individual cases with liver unit team
Nutrition
- Seek nutritional review and ongoing nutritional advice from neonatal/liver dietitian
- If baby acutely unwell stop all enteral feeds until galactosaemia excluded. Otherwise, continue mother’s own breast milk, as available, +/- breast milk fortifier or preterm or term formula (as appropriate) while baby achieves adequate growth velocity
Babies with faltering growth
| Milk available | Preterm baby (<36 weeks) | Term baby (>2 kg) |
| Breast | Replace 25–50% feeds by volume with concentrated Aptamil® Pepti Junior* | Replace 25–50% feeds by volume with Infatrini® Peptisorb |
| Formula | Replace 25–50% feeds by volume with concentrated Aptamil® Pepti Junior | Replace all formula with Aptamil® Pepti Junior |
Concentrated Aptamil® Pepti Junior (16%)
- Add 4 level scoops Aptamil® Pepti Junior to 100 mL of cooled, boiled water and mix well
- Store in fridge until use, discard unused feed after 12 hr
- Per 100 mL: 79 kcal, 2.16 g protein, 1 mmol sodium
- If conjugated bilirubin >50 and baby not receiving parenteral lipid >10 mL/kg/day start fat soluble vitamins in doses below:
- vitamin K: 300 micrograms/kg oral (IV if acute liver failure) daily: monitor PT and APTT
- vitamin A: 1000 units/kg (rounded to nearest 1000 units)
- ergocalciferol 400–800 units/kg/day
- vitamin E: alpha-tocopherol 10 mg/kg/day
- DO NOT give ABIDEC or Dalavit alongside fat soluble vitamins A, D, E, K
Ursodeoxycholic acid
- 10 mg/kg twice daily
Parenteral nutrition
- Wherever possible, feed enterally, as even small amounts have trophic effects on gut, reduce bacterial colonisation and promote bile flow
- Bolus feeds promote bile flow more readily than continuous feeds, but the latter may be better absorbed
- Refer to neonatal/paediatric or network dietitian for advice in babies who fail to make enteral progress
- If direct bilirubin >50 micromol/L, consider switching to SMOF lipid
- Discontinue PN as soon as possible in all preterm babies with cholestasis
Specific treatments
- Babies with cystic fibrosis, galactosaemia, tyrosinaemia type 1, hypopituitarism, hypothyroidism or bile acid disorders require additional targeted management and life-long follow-up shared by local teams and appropriate specialists
FOLLOW-UP
- For babies with persistent cholestasis, arrange outpatient follow-up with liver team after discharge from NNU
- If liver dysfunction has resolved, no follow-up with liver team necessary
- For all others with a specific diagnosis, follow-up will be directed by liver team, appropriate specialists and local consultant
- Long-term hepatic outcome for multifactorial preterm or neonatal hepatitis is excellent, majority resolve within first year
Date updated: 2024-02-26