INTRODUCTION
- Discomfort, pain or stress can be associated with routine care and invasive procedures. Babies are unable to report pain; use observational skills and clinical judgment
Key recommendations
- Routine assessments to detect pain using a validated assessment tool
- Minimise number of painful procedures
- Prevent/reduce acute pain from invasive procedures using non-pharmacological and pharmacological methods
- Anticipate and treat post-operative pain
Types of pain
| Acute pain | Skin-breaking procedures or tissue injury caused by diagnostic or therapeutic interventions |
| Established pain | Occurs after surgery, localised inflammatory conditions, birth-related trauma |
| Prolonged/chronic pain | Results from severe diseases e.g. necrotising enterocolitis (NEC), meningitis. Pathological pain state persisting beyond normal tissue healing time |
Symptoms and signs
- Lack of behavioural responses does not exclude pain
| Physiological changes | Behavioural changes | Anatomical changes |
Body movements |
|
|
|
|
- Sudden pain and distress may indicate acute deterioration e.g. bowel perforation
- Physiological changes cannot be sustained long-term
PAIN ASSESSMENT
- Assess within 1 hr of admission
- Frequency of further assessments will depend on baby’s clinical condition, underlying diagnosis and pain score (see Frequency of assessment below)
Pain assessment tools
- Separate tools may be needed to assess acute and prolonged pain
- Use validated pain assessment tools [Pain Assessment Tool (PAT) and Premature Infant Pain Profile (PIPP)]
- See Abstinence syndrome guideline for assessment of babies with neonatal abstinence syndrome
Pain assessment not indicated/unsuitable
| Not indicated | Unsuitable |
|
|
Use of pain assessment tool
- Note gestational age
- Observe baby’s behaviour for 15–30 sec then gently touch baby’s limb to determine muscle tone/tension (can be done during routine handling)
- Note:
- physiological conditions that may influence score (in cyanotic heart disease, baby’s colour may score normal unless there is a change in the intensity of the cyanosis or duskiness due to pain)
- medications that may affect behaviour or physiological responses
- environmental triggers (sudden bright lights, noise, activity) may cause a stress response. Document on chart or in notes at time of score
- When score is above tool’s recommended thresholds, initiate comfort measures or analgesia
Frequency of assessment
- All babies to have pain assessment within 1 hr of admission
- Minimum frequency of subsequent assessments depends on level of care
- intensive care: hourly with observations
- high dependency: 4-hrly
- special care: as condition dictates
- post-operatively: hourly for first 8 hr, then 4-hrly until 48 hr post-op (more frequently if signs of distress/discomfort)
- If baby shows signs of distress/discomfort perform additional assessments
PAIN MANAGEMENT
Indications
- Birth trauma
- Iatrogenic injury
- Before, during and after any painful procedure
- Severe illness e.g. NEC, meningitis
- To aid ventilation
- Preparation for transfer if ventilated
- Whilst undergoing therapeutic hypothermia
- Post-operatively
- End-of-life care
- Formal assessment indicates pain
- If non-pharmacological techniques are ineffective or not appropriate, progress to pharmacological agents (e.g. post-surgery, severe illness, major injury, congenital malformations and palliative care)
Non-pharmacological pain relief
- Gently repositioning baby
- Light swaddling (blanket/nest), prolonged restrictive swaddling may be associated with increased risk of developmental hip dysplasia
- Comfort/containment holding
- Reducing light, noise, and activity around baby
- Soothing voice
- Nappy change
- Non-nutritive sucking (NNS) (dummy or gloved finger) [see Non-nutritive sucking (NNS) guideline]
- Kangaroo care (see Kangaroo care guideline)
- Breastfeed (see Breastfeeding guideline)
- Sucrose
- Mother’s expressed breast milk (MEBM) – no additives
Reassess after 30 min
- If pain score in upper range, institute comfort measures and administer prescribed analgesia/seek medical review
- If score continues to rise, consider increasing dose of analgesia and reassess after 30 min
- if clinical concerns – medical review
- If score constantly below baseline and analgesia maintained, reduce dosage
- Record effectiveness of pain management in care plan
Sucrose
- Sucrose 24% solution and breast milk provide a quick, short-term analgesic effect (given orally)
- NNS increases effectiveness
- Use in conjunction with environmental and behavioural measures to relieve pain (e.g. positioning, swaddling, containment holding, kangaroo care)
- may be given to ventilated babies with care
Contraindications to sucrose
| Do not use | May not be effective |
|
|
Administration
- Use commercially available sucrose 24% solution and follow manufacturer’s guidelines regarding storage and use
- Maximum 8 doses in 24 hr
- Avoid risk of choking/aspiration – ensure baby is awake
- Drop dose onto tongue, buccal membrane, or dummy and wait 2 min before starting procedure
- For procedures lasting >5 min, repeat dose (maximum 2 further doses)
- Continue environmental and behavioural management strategies during procedure
- Observe baby's cues and allow ‘time-out’ to recover
- Document administration of sucrose as per local policy
| Gestation | Dose of sucrose 24% |
| 28+0–30+6 weeks | 0.1 mL (max 0.3 mL per procedure) |
| ≥31+0 weeks and 1000–2000 g | 0.2 mL (max 0.6 mL per procedure) |
| >2000 g | 0.5 mL (max 1.5 mL per procedure) |
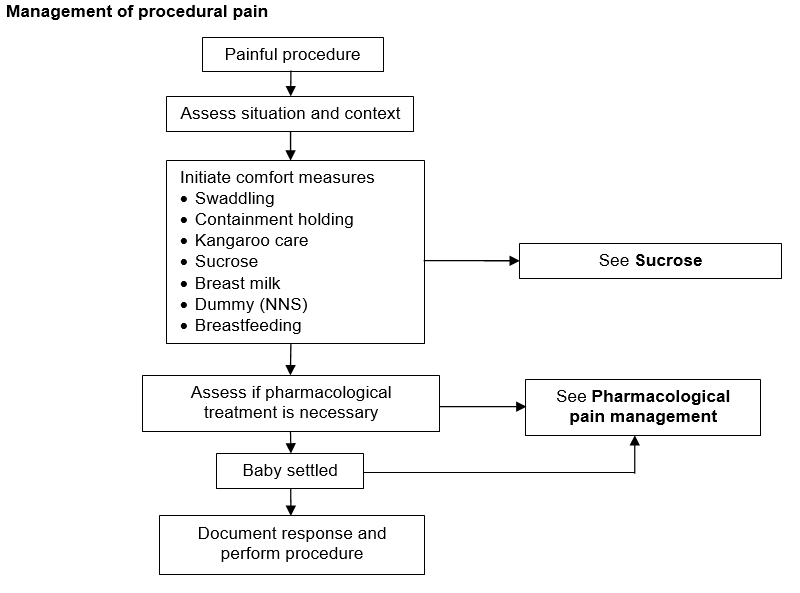
Management of procedural pain
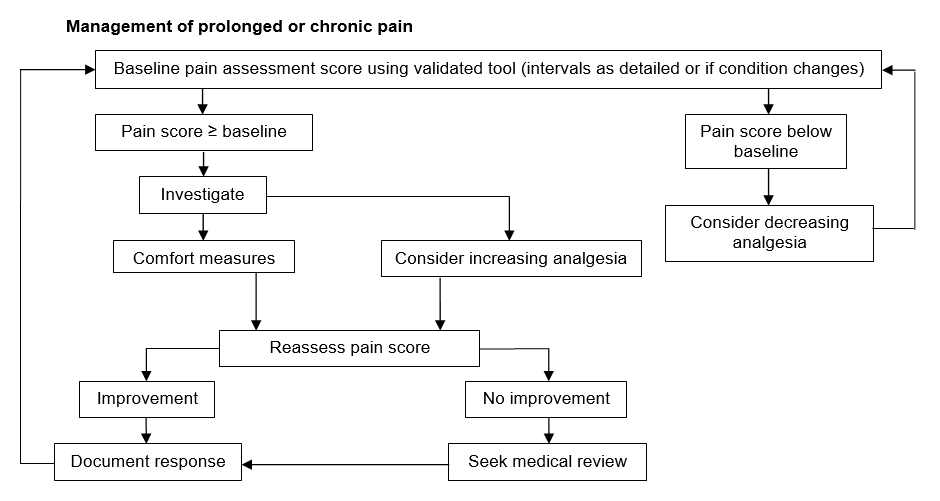
Management of prolonged or chronic pain
Pharmacological pain management
- Give medication in conjunction with non-pharmacological measures
- The following drugs may be useful:
- diamorphine
- fentanyl
- morphine
- paracetamol
- Details of these drugs can be found in the Neonatal Formulary
Suggested medication for procedures
Specific situations
| Non-urgent endotracheal intubation | Mechanical ventilation |
Chest drain insertion |
CT/MR imaging |
Laser therapy for ROP | Therapeutic hypothermia |
|
|
|
|
|
|
Simple surgical procedures
| Abdominal drain insertion | Broviac line removal | Wound dressing/drain removal | Application of silo bag for gastroschisis |
|
|
|
|
Date updated: 2024-02-05