INTRODUCTION
- Supraventricular tachycardia (SVT) is the most common pathological tachycardia in newborns – can be new presentation or commenced in fetal life
RECOGNITION AND ASSESSMENT
- Sustained, accelerated non-sinus rhythm, regular and narrow-complex, originating above the level of the atrioventricular (AV) junction
- Heart rate >200 bpm
- May be 1 of 3 tachycardias:
- atrial
- atrioventricular nodal re-entry (AVNRT)
- atrioventricular re-entrant (AVRT) – most common SVT in fetal and neonatal life
- Can be presenting feature of a congenital heart defect – but do not wait to exclude this before commencing treatment
SYMPTOMS AND SIGNS
- Can be variable with some common presentations:
- acute onset in a baby in heart failure/shock with no previous signs and symptoms
- fetal tachycardia during pregnancy
- baby with irritability, poor feeding, sweating and breathlessness for hours/days before presentation
- SVT can cause reduced cardiac output due to reduced diastolic filling time
- many babies tolerate SVT well, however if tachycardia is sustained for >6 hr signs of congestive heart failure may develop, with irritability, tachypnoea and pallor
CAUSES
- No known cause in majority of babies
- Idiopathic SVT is more common in neonates than older children
- Wolf-Parkinson-White pre-excitation – only becomes visible after conversion to sinus rhythm
- Congenital heart defect, including Ebstein’s and TGA
TRIGGERS
- Co-existing infections e.g. LRTI
- Manage all triggers appropriately
EXAMINATION
- Heart rate: >200 bpm
- Capillary refill
- Blood pressure
- Respiratory rate, may be normal/abnormal depending on:
- signs of heart failure
- co-existing respiratory conditions
- infections
- SpO2 may be normal, low, or of poor signal in haemodynamic compromise
- Cardiovascular and respiratory examination; may be normal aside from fast heart rate
- Examine baby for other reasons of tachycardia, including pain and environmental factors e.g. pyrexia (particularly in premature baby in incubator)
INVESTIGATIONS
- 12-lead ECG to confirm SVT diagnosis in haemodynamically stable cases
- if baby haemodynamically unstable, or if ECG not available, defibrillator can record and print rhythm strips from 3 different leads
- Once SVT terminated, perform repeat ECG to assist with identification of pre-excitation and any other underlying rhythm abnormality
- Blood gas for:
- acid-base balance
- electrolytes
- ionised calcium
- Echocardiogram to assess structural anatomy and cardiac function
MANAGEMENT
Contact cardiology team as soon as baby is deemed unstable
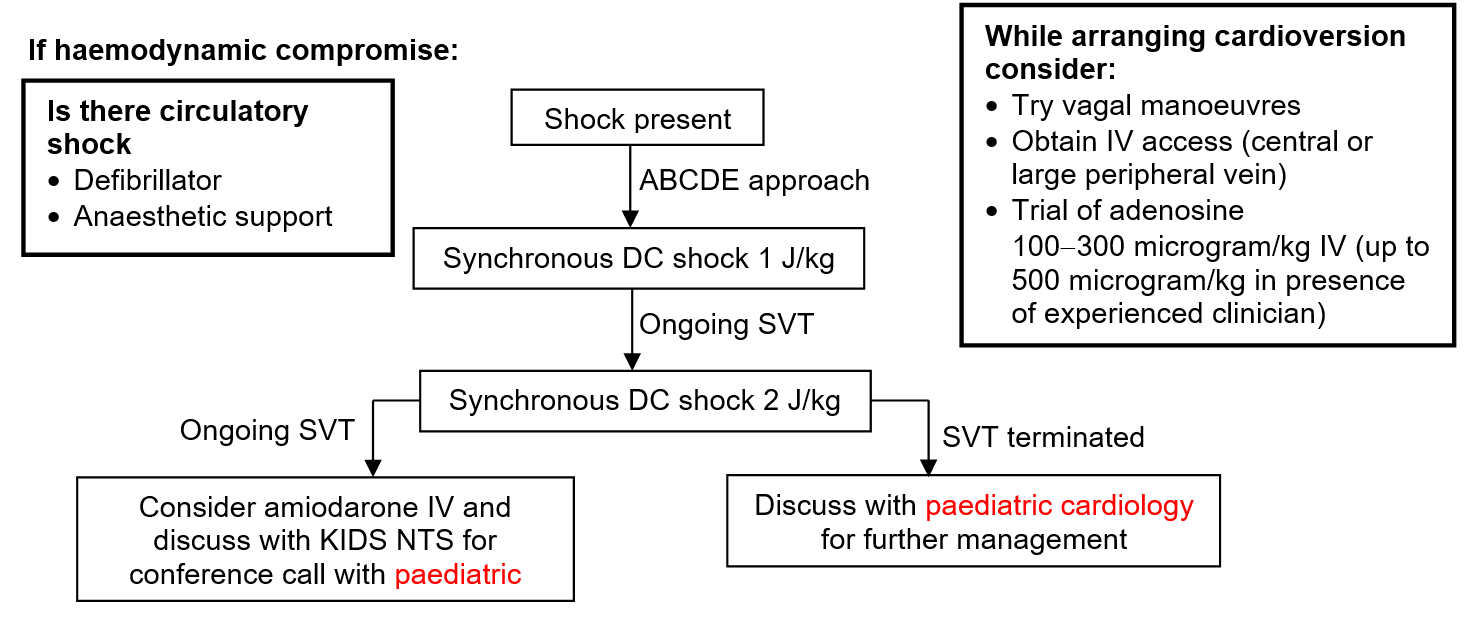
If haemodynamic compromise:
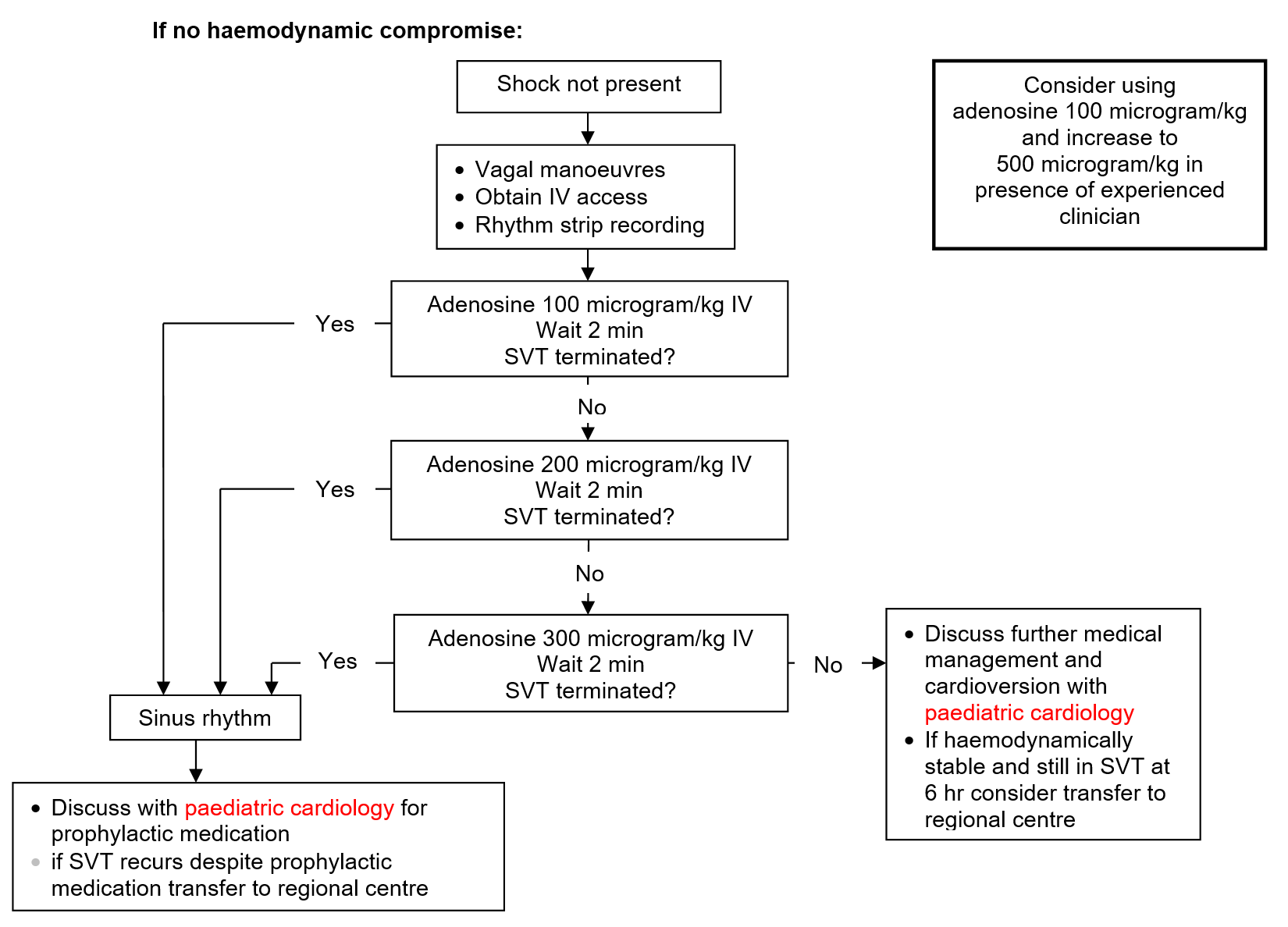
If no haemodynamic compromise:
ADDITIONAL INFORMATION
Adenosine
- Give via cannula into large vein in upper limb, followed by rapid sodium chloride 0.9% flush; very short half-life of 10–30 sec – must get to the heart as quickly as possible
- Acts by slowing conduction time through the AV node
- Intraosseous access ineffective due to time taken for venous return
- Use 3-way tap with Luer-lock syringes; 1 syringe for adenosine and 1 for sodium chloride 0.9% flush
Never test cannula by aspirating blood into syringe with adenosine before injection – will lead to breakdown of adenosine
Major route of elimination via active take-up by red blood cells and vascular endothelial cells where it is metabolised
Major route of elimination via active take-up by red blood cells and vascular endothelial cells where it is metabolised
- Keep defibrillator nearby
- Capture and print rhythm, while adenosine given, via defibrillator rhythm strip or ECG recording
- Starting dose 100 microgram/kg, repeat after 2 min, if no effect increase to maximum dose of 300 microgram/kg as in flowchart above
- if experienced clinician present, maximum dose 500 microgram/kg
Vagal manoeuvres
- Cold stimulation of the trigeminal nerve (afferent branches) leads stimulation of the vagal nerve (efferent branches); slows AV node conduction
- wrap bag of ice in towel and apply to baby’s face or
- wrap baby in towel and immerse entire head in ice-cold water for 5 sec
- Unilateral carotid massage not recommended – difficult to perform in neonates and has limited effect
DC cardioversion
- Applies direct current of electricity to the heart, synchronised to R wave of QRS complex on ECG
- less risk of inducing ventricular fibrillation than unsynchronised
- Ideally carry out under general anaesthetic, or at least sedation
- If performed outside NNU, will require anaesthetic support
- Synchronised shock starting at 1 J/kg, if no response increase to 2 J/kg as in flowchart above
Chemical cardioversion
- Discuss with paediatric cardiology if:
- haemodynamically unstable and unresponsive to adenosine IV or DC cardioversion
- haemodynamically stable and unresponsive to adenosine IV
- If SVT occurred in-utero consult perinatal plan and discuss with paediatric cardiology
Prophylactic medication
- When SVT has terminated, it is vital to commence medication to prevent further episodes
- Choice of prophylactic medication based on:
- previous history of SVT (including in fetal life)
- assessment of ECG, both in SVT and once terminated
- cardiac function
- Discuss with paediatric cardiology centre and send ECG/echocardiogram for review
FOLLOW-UP
- Any episode of SVT – follow-up with paediatrician with expertise in cardiology/paediatric cardiologist
- Arrange:
- baseline echocardiogram in outpatient clinic (if not already done)
- Holter monitor
Date updated: 2024-01-09