INTRODUCTION
- 40% of maternal untreated early syphilis results in stillbirth/spontaneous abortion/perinatal loss
- Risk of baby being affected depends on the staging of maternal infection, which includes:
- time of infection
- treatment completion
- Majority of adverse outcomes occur in those with no antenatal screening or inadequate maternal treatment
- Congenital syphilis can be divided into early (aged <2 yr) and late disease (aged >2 yr)
- Babies born to mothers diagnosed and treated during current pregnancy require serological testing after birth
RECOGNITION AND ASSESSMENT
- Clarify maternal treatment and post-treatment titres
- Discuss management plan with parents before birth
- All parents to be seen by specialist midwife antenatally to discuss management of baby
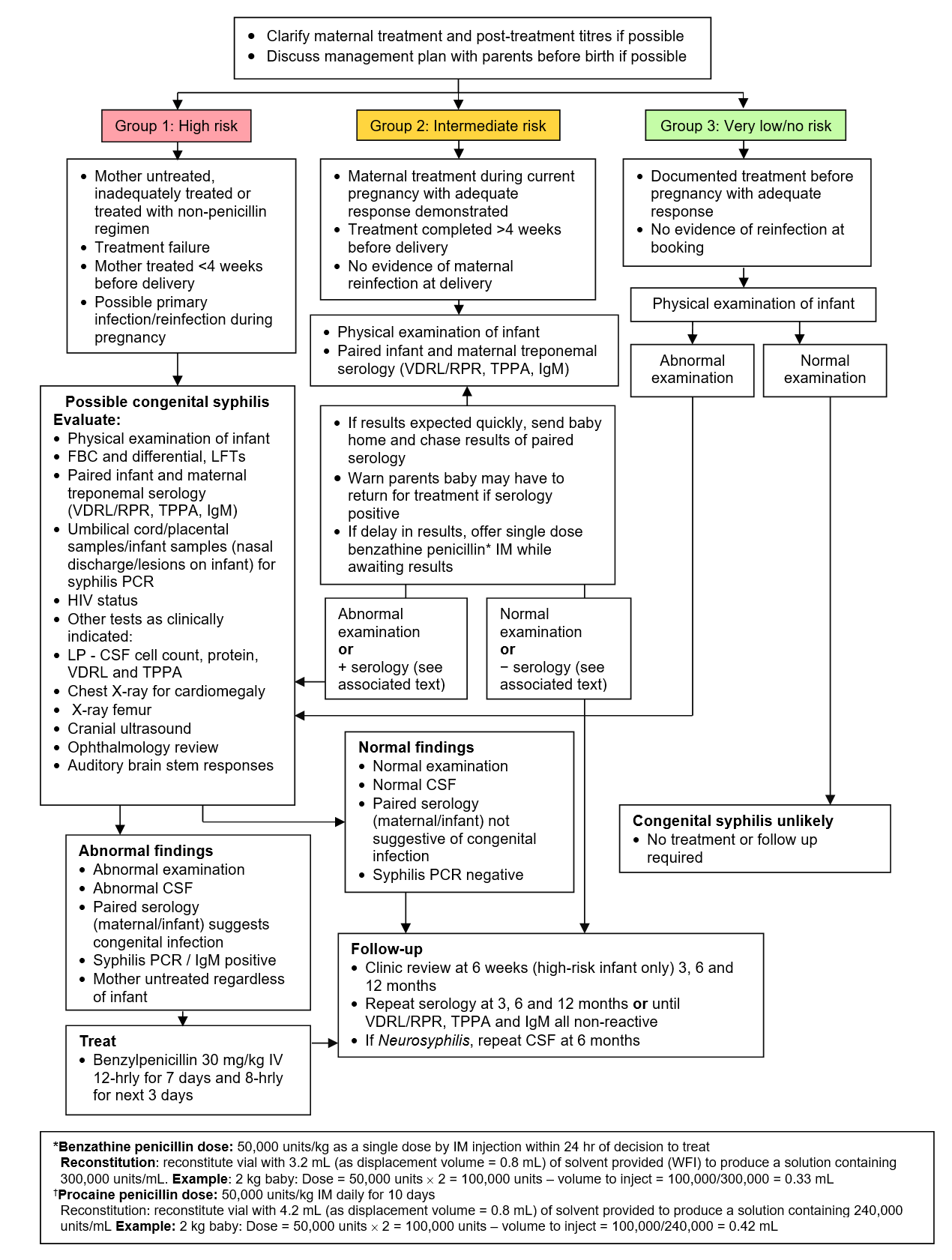
- Follow Management flowchart
Management flowchart: Baby born to mother with positive syphilis serology (IgM/VDRL/RPR or TPPA reactive)
CLINICAL FEATURES
Early congenital syphilis
- Symptoms represent active infection and inflammation, but 2/3 of infected babies will be asymptomatic at birth
- Rash
- Infectious snuffles (copious nasal secretions)
- Haemorrhagic rhinitis
- Osteochondritis
- Periostitis
- Pseudo-paralysis
- Mucocutaneous patches
- Peri-oral fissures
- Hepatosplenomegaly
- Lymphadenopthy
- Oedema
- Glomerulonephritis
- Ocular or neurological involvement
- Haemolysis
- Thrombocytopenia
Late congenital syphilis
- Symptoms represent response to early infection and chronic inflammation. These features are not present at birth and some may only become apparent in early adolescence
- CNS disease (VIII nerve deafness)
- Bone and joint (frontal bossing, saddle nose, high palate and Clutton joints)
- Teeth (Hutchinson incisors and mulberry molars)
- Eye (interstitial keratitis 5–20 yr) involvement
ASSESSMENT OF MATERNAL TREATMENT
- Local GUM team to advise if maternal serology confirms previous adequately treated syphilis, or suggests new/reinfection
- treatment is adequate if completed >30 days before delivery and if plasma reagin (RPR)/venereal disease research laboratory (VDRL) titre was detectable at diagnosis, it fell rapidly
- All babies born to mothers with positive treponemal serology require clinical evaluation and syphilis serology tests except babies born to mothers who had syphilis cured before current pregnancy
- mothers of babies who do not require testing will be IgM negative, RPR/VDRL test negative, Treponema pallidum particle agglutination (TPPA) test positive
- GUM team will classify baby as ‘very low risk’, ‘intermediate risk’ or ‘high risk’ depending on:
- maternal treatment
- interval between treatment and birth
- maternal RPR/VDRL
- risk of re-infection from untreated partner
- recurrent clinical signs
INVESTIGATIONS
Diagnostic serology
- Baby may have positive serology depending on timing of maternal infection, therefore mother must be screened simultaneously for titre comparison. Serological tests must be performed on baby’s blood, DO NOT USE CORD BLOOD
Non-treponemal tests
- VDRL/RPR detects biomarkers from cells damaged by syphilis spirochaete
- reflects current disease activity, falls in response to adequate treatment
- 4 x decrease in titre = effective treatment
- 4 x increase after treatment = relapse or reinfection
- May be false negative in babies who acquire congenital syphilis in late pregnancy or have extremely high antibody titres before dilution (prozone phenomenon)
- May be false positive in viral infections (Epstein-Barr, varicella zoster, hepatitis, measles), tuberculosis, endocarditis, malaria, lymphoma, connective tissue disease, pregnancy, intravenous drug use
Treponemal tests
- Syphilis IgM
- Direct antibody to the syphilis spirochate; positive in early infection and falls slowly (aged >2 yr)
- does not cross the placenta so is a good marker for congenital syphilis infection if positive in baby
- TPPA
- Treponema pallidum haemagglutination assay (TPHA)
- Fluorescent treponemal antibody absorption test (FTA-ABS)
- Tests may also be positive in other spirochetal disease e.g. leptospirosis, and Lyme disease. There is poor correlation of titres with disease activity
Interpretation of syphilis serology of baby
- Following indicate congenital infection:
- positive syphilis IgM
- positive RPR/VDRL test on CSF
- ≥4 x difference of RPR/VDRL titre or TPPA titre above that of the mother
- ≥4 x increase in RPR/VDRL or TPPA titre within 3 months of birth
- positive treponemal tests in child aged >18 months
Example of positive TPPA
- Maternal titres 1:1024
- Baby serology 1:4096 (i.e. baby 4 x greater than mother)
Example of positive VDRL/RPR
- Maternal titres 1:64
- Baby serology 1:256 (i.e. baby 4 x greater than mother)
CSF
- CSF investigations require ≥0.5 mL of CSF. A CSF is classed as positive if:
- increased WCC and protein
- reactive TPPA and VDRL (a negative VDRL does not exclude neurosyphilis)
- Remember to suspect other causes of elevated values when evaluating baby for congenital syphilis
TREATMENT
- Possible congenital syphilis: benzylpenicillin 30 mg/kg IV 12-hrly for 7 days and 8-hrly for next 3 days
- †Alternative regimen (if, for example, difficulty with IV access): procaine benzylpenicillin 50,000 units/kg daily IM for 10 days (painful)
- If treatment interrupted for >1 day course must be restarted
- *If delay in results, offer single dose benzathine benzylpenicillin IM while awaiting results:
- 50,000 units/kg as a single dose by IM injection within 24 hr of decision to treat
FOLLOW-UP
- If IgM test is negative, other tests are reactive with titres <4-fold higher than mother’s, with no signs of congenital syphilis, repeat reactive tests at 3, 6 and 12 months or until all tests (VDRL/RPR, TPPA and IgM) become negative (usually by 6 months)
- If baby’s serum negative on screening, and no signs of congenital infection, no further testing necessary
- If any doubt regarding test interpretation/follow-up, discuss with local expert in neonatal infection/microbiology
- If Neurosyphilis, repeat CSF at 6 months
Date updated: 2024-01-16