DEFINITION
- Platelet count <150 x 109/L
- mild (platelet count 100–150 x 109/L) and moderate (50–100 x 109/L) thrombocytopenia occur frequently in preterm babies who are ill, and in those born to women with pregnancy-induced hypertension (PIH)
- severe thrombocytopenia (<50 x 109/L) is uncommon, particularly in apparently healthy term babies and raises the possibility of neonatal allo-immune thrombocytopenia (NAIT; see below)
- ensure results are not spurious, if in doubt repeat venous sample
CAUSES
| WELL | ILL | |
| Common |
|
|
| Rare |
|
|
Severe thrombocytopenia in an otherwise healthy term newborn baby is NAIT until proved otherwise
INVESTIGATIONS
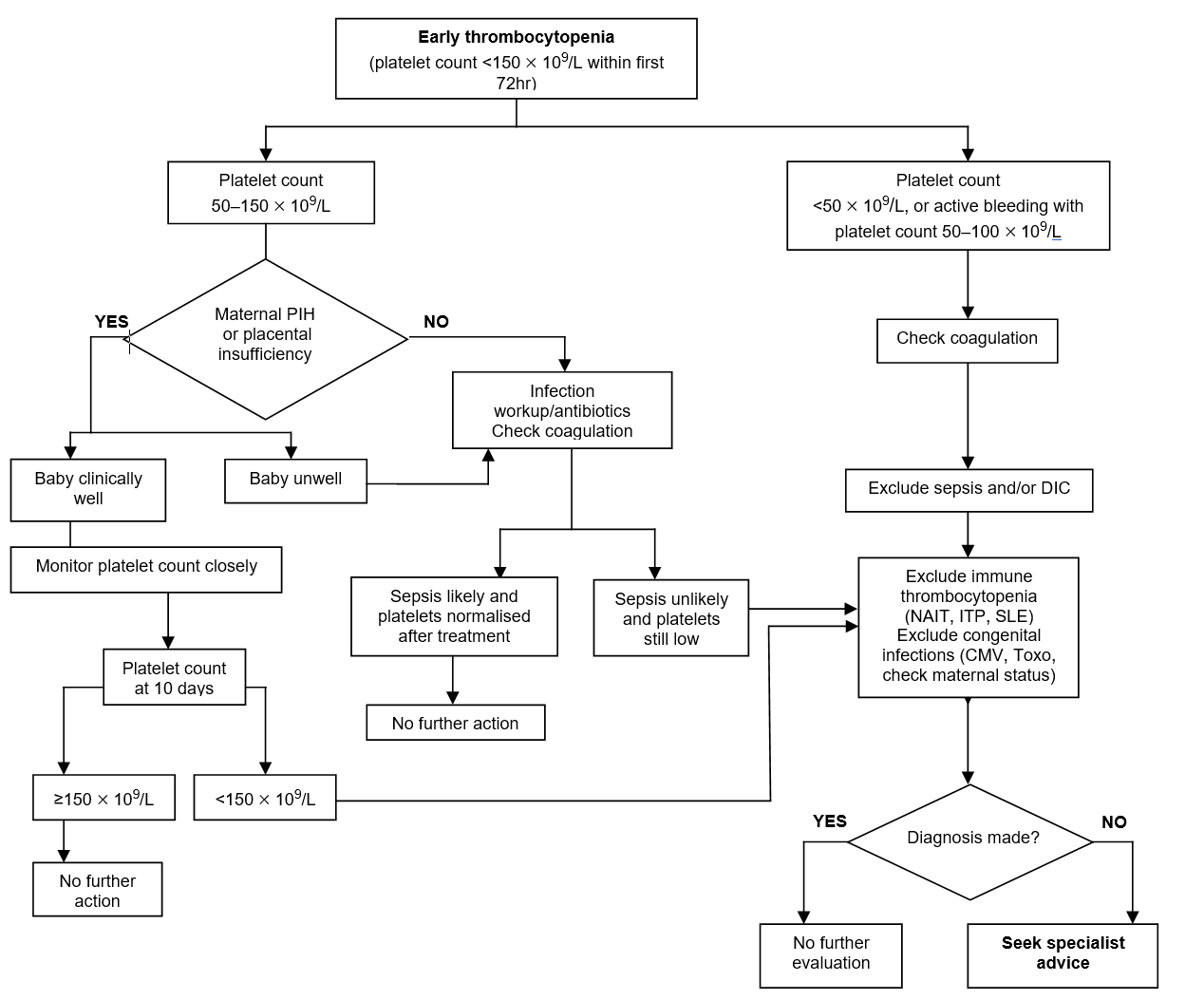
- Evaluation of early-onset (<72 hr after birth) thrombocytopenia (see Flowchart)
- preterm babies with early-onset mild-to-moderate thrombocytopenia in whom there is good evidence of placental insufficiency: further investigations not warranted unless platelet count does not recover within 10–14 days
- preterm babies without placental insufficiency: investigate first for sepsis
- term babies: investigate for sepsis and NAIT
- If severe thrombocytopenia, perform clotting screen
- Look for presence of active bleeding or visible petechiae
- If features suggestive of congenital infection (e.g. abnormal LFT, rashes, maternal history etc.) or if persistent or unexplained thrombocytopenia, perform congenital infection i.e. CMV and toxoplasma serology; check maternal status for syphilis, rubella and HIV; herpes simplex and enteroviral screen
- Obstetric history, particularly maternal platelet count, drugs, pre-eclampsia. Family history of bleeding disorders
- Careful examination, include other associated features (e.g. trisomies and inherited syndromes)
Evaluation of late onset thrombocytopenia
- Thrombocytopenia presenting in baby after first 3 days of life, presume underlying sepsis or NEC until proved otherwise
- these babies are at significant risk of haemorrhage, though the benefit of platelet transfusion is not clear-cut
Summary of investigations (also refer to text above)
MANAGEMENT
General
Avoid
- Heel prick and IM injections, use venepuncture and IV injections
- Invasive procedure (central line, LP, chest drain etc.). If any of above are unavoidable:
- discuss with on-call consultant
- give platelet transfusion if platelet count <50 x 109/L before the procedure (if semi-elective e.g. LP, central lines) or during/soon after procedure (if emergency e.g. chest drain)
- give particular attention to haemostasis
Platelet transfusion
- Only available for immediate and specific therapy for thrombocytopenia but carries risk of transfusion-related infections and transfusion reactions, and only after discussion with consultant
Indications for platelet transfusion (term and preterm babies)
- Main objective is to prevent consequences of severe thrombocytopenia, significant risk of acute intracerebral haemorrhage and neuromorbidity
Platelet count <25 x 109/L
- In otherwise well baby, including NAIT, if no evidence of bleeding and no family history of intracranial haemorrhage
Platelet count <50 x 109/L
- In baby with:
- clinical instability
- concurrent coagulopathy
- birth weight <1000 g and aged <1 week
- previous major bleeding e.g. intraventricular haemorrhage (IVH)
- current minor bleeding (e.g. petechiae, venepuncture oozing)
- planned surgery, exchange transfusion or invasive procedure (central line insertion, LP, chest drain, ECMO etc.)
- platelet count falling and likely to fall below 30
- NAIT if previously affected sibling with intracranial bleed
- PDA treated with indomethacin or ibuprofen
Platelet count <100 x 109/L
- If major bleeding or major surgery (e.g. neurosurgery), give platelet transfusion
Type of platelets
- NAIT: HPA compatible platelets wherever possible
- All others: blood group-compatible CMV negative
- Irradiation of platelets is not routinely required but consider for babies with definite or suspected immunodeficiency, or those who have undergone intrauterine transfusions
Volume of platelets
- 10–20 mL/kg (10 mL/kg usually raise platelet count by >50 x 109/L). Babies with suspected NAIT will require higher dose of 20 mL/kg
ADMINISTRATION OF PLATELETS
Never administer platelets through an arterial line or UAC
- Use platelets as soon as they arrive on ward (ensure IV access before requesting platelets from blood bank)
- Keep platelets at room temperature
- To minimise loss, draw contents of pack into 50 mL syringe through a special platelet or fresh blood transfusion set with a 170–200 micrometre filter and infuse, using a narrow bore extension set linked to IV line, primed with sodium chloride 0.9%
- Transfuse platelets over 30–60 min, mixing syringe from time to time to avoid platelets settling down
- There is no need for routine use of diuretic after platelet transfusion
- Check platelet count within 12 hr after transfusion
NAIT
- Analogous to rhesus haemolytic disease and caused by transplacental passage of maternal alloantibodies directed against fetal platelet antigens, inherited from father but absent in mother
- Majority caused by antibodies against platelet antigens, HPA-1a (80%) and HPA-5b (10–15%)
- NAIT can affect first pregnancy and has 10% risk of severe intracranial haemorrhage; 20% of survivors exhibit significant neurodevelopmental sequelae
Recognition
- For HPA-1a antigen-negative women, complete a neonatal alert form
- Petechiae, purpura, excessive bleeding and severe thrombocytopenia in an otherwise healthy term newborn baby indicate NAIT until proved otherwise
- NAIT can also present with:
- fetal intracranial haemorrhage or unexplained hydrocephalus
- postnatal intracranial haemorrhage in term baby
If NAIT suspected, involve consultant neonatologist immediately
Assessment
- Check baby’s platelet count daily until >100 x 109/L
- Check mother’s platelet count (may already be in maternal healthcare record)
- Obtain blood from mother, baby and father for platelet typing and antibodies. Liaise with haematology department about appropriate samples
- Arrange cranial ultrasound scan (see Cranial ultrasound scans guideline)
Treatment
- In 30% of cases, maternal antibody may not be found and can be detected later
- Transfuse baby with suspected NAIT with accredited HPA-1a antigen-negative platelets if:
- bleeding or
- platelet count <25 x 109/L
- National Blood Service has a pool of suitable donors, and platelets are available at short notice from blood bank
- if accredited HPA-1a negative platelets not available, administer random donor platelets
Inform blood bank and consultant haematologist as soon as NAIT suspected.
Do not delay transfusion for investigations
- If thrombocytopenia severe (<50 x 109/L), or haemorrhage persists despite transfusion of antigen-negative platelets, administer intravenous human immunoglobulin (IVIG) 1 g/kg/day once daily (give 1 full 2.5 g vial maximum for babies ≥2.5 kg) for 1–3 days (may require additional doses 2–4 weeks later)
- Aim to keep platelet count >25 x 109/L for first week of life, or as long as active bleeding continues
- Report newly diagnosed babies with NAIT to fetal medicine consultant for counselling for future pregnancies
NEONATAL AUTOIMMUNE THROMBOCYTOPENIA
Clinical features
- Caused by transplacental passage of autoantibodies in women with ITP or SLE, and affecting about 10% of babies born to such women
- Severity generally related to severity of maternal disease
- Risk of intracranial haemorrhage in baby <1%
Management
- Report all women with thrombocytopenia and those splenectomised through Neonatal Alert System, and instigate plan of management
- Send cord blood for platelet count
- Check baby’s platelet count 24 hr later, irrespective of cord blood result
- If baby thrombocytopenic, check platelet count daily for first 3–4 days or until >100 x 109/L
- If platelet count <25 x 109/L, whether bleeding or not, treat with IVIG (dose as in NAIT) +/-steroids
- Discharge baby when platelet count >100 x 109/L
- For babies requiring IVIG, recheck platelet count 2 weeks later. A few may require another course of IVIG at this time because of persistence of maternal antibodies
Date updated: 2024-02-26