RECOGNITION AND ASSESSMENT
- Obstetric team should inform neonatal team after delivery of a baby with maternal history of hyperthyroidism (Graves’ disease) or hypothyroidism
MATERNAL HYPERTHYROIDISM
Common
- Maternal Graves’ disease (autoimmune hyperthyroidism)
- IgG thyroid stimulating antibodies cross from mother with Graves’ disease to fetus towards the end of approximately 1 in 8 pregnancies
- half-life of thyroid stimulating antibodies is approximately 12 days and resolution of fetal thyrotoxicosis corresponds to their degradation over 3–12 weeks
Rare
- Maternal Hashimoto’s thyroiditis producing thyroid stimulating antibodies
- Activating mutations of TSH receptor (family history of hyperthyroidism in first degree relatives)
Babies at high risk
- Mother has high levels of thyroid antibodies [thyroid stimulating immunoglobulin (TSI) or thyroid receptor antibody (TRAb)] – refer to maternal healthcare record
- Maternal thyroid antibody status unknown
- Mother clinically hyperthyroid or receiving antithyroid drugs in third trimester
- Mother previously treated with radioactive iodine or surgery or with previously affected babies
- Evidence of fetal hyperthyroidism
- Family history of TSH receptor mutation
Clinical features of fetal hyperthyroidism
- Usually present by aged 24–48 hr but can be delayed up to 10 days. Disorder is self-limiting over 3–12 weeks, although there may be some longer-term neurological defects
- Head and neck
- goitre, periorbital oedema, exophthalmos
- Central nervous system (CNS)
- irritability, jitteriness, poor sleeping, microcephaly
- Cardiovascular system (CVS)
- tachycardia, arrhythmias, flushing, sweating, hypertension
- Gastrointestinal (GI)
- diarrhoea, vomiting, excess weight loss, hepatosplenomegaly
- Others
- bruising, petechiae due to thrombocytopenia, jaundice
It is not sufficient to judge risk based on current maternal thyroid function as mothers on antithyroid medication or who have received thyroid ablative therapy (surgery or radioactive iodine) may be euthyroid or hypothyroid yet still have high thyroid antibody titres
Management
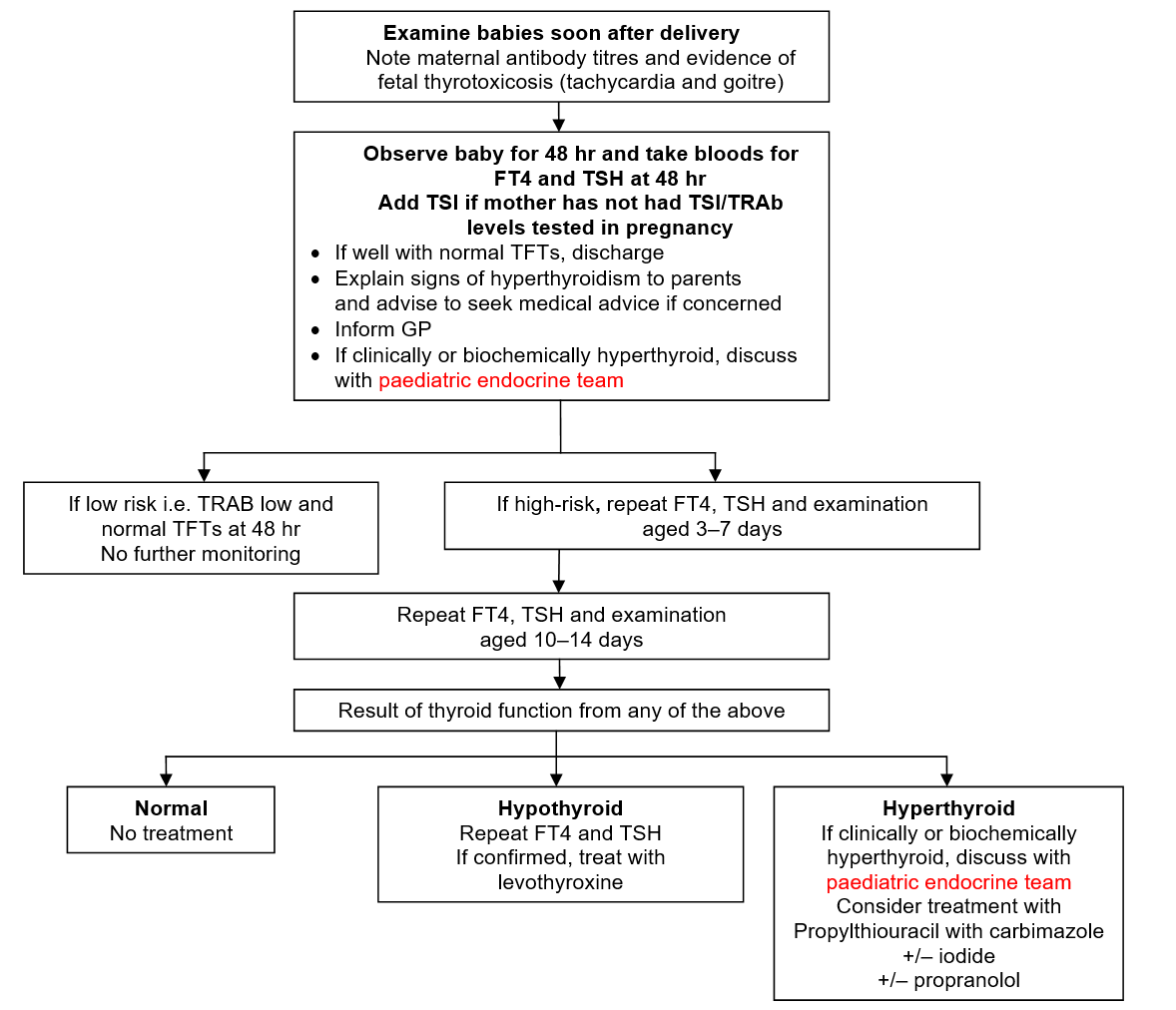
- Follow Management flowchart
- Examine high-risk babies after delivery
- note maternal antibody titres and evidence of fetal thyrotoxicosis (tachycardia and goitre)
- Observe baby for 48 hr and take bloods for FT4 and TSH at 48 hr
- if well with normal TFTs, (see Hypothyroidism guideline for normal values) discharge
- Explain signs of hyperthyroidism to parents and advise to seek medical advice if concerned
- If baby high risk, repeat TFTs at 3–7 days and arrange review at 10–14 days to repeat TFTs and clinical assessment
- If low risk, i.e. TRAb levels low, if TFTs normal at 48 hr no further repeats needed
- If at any stage clinically or biochemically hyperthyroid, discuss with paediatric endocrine team
Flowchart: Management of babies at risk for congenital hyperthyroidism
MATERNAL HYPOTHYROIDISM
Physiology
- After onset of fetal thyroid secretion at mid-gestation, maternal transfer of T4 continues to contribute to fetal serum T4, protecting neurodevelopment until birth. Prompt treatment of maternal hypothyroidism should mitigate negative effects on baby’s neurodevelopment
Risks associated with maternal hypothyroidism
- Preterm delivery
- Intrauterine growth restriction
- Postpartum bleeding
- Untreated severe hypothyroidism in mother can lead to impaired brain development in baby
Management
- Hashimoto’s thyroiditis (autoimmune) occurs in approximately 2.5% of women and is associated with thyroid inhibiting or, rarely, thyroid stimulating antibodies. Baby may develop transient hypo or, rarely, hyperthyroidism. These babies should be reviewed at 10–14 days and have their T4/TSH checked
- Babies born to mothers with congenital hypothyroidism (aplasia/hypoplasia) and treated with levothyroxine do not require routine thyroid function testing
- Mothers who have been treated for Graves’ disease (surgery or radioactive iodine) may be euthyroid or hypothyroid but may still have high thyroid antibody. Treat as high risk for neonatal hyperthyroidism and follow guideline for maternal hyperthyroidism
Breastfeeding
- Encourage for all babies even if mother currently taking carbimazole, propylthiouracil or levothyroxine
Contraindication
- Radioactive iodine treatment
Date updated: 2024-02-05