Adapted with permission, Guy's and St Thomas’ NHS Trust nursing guideline
INTRODUCTION
- In babies requiring assisted ventilation, it is essential to monitor arterial partial pressure of oxygen (PaO2) and carbon dioxide (PaCO2) to ensure adequate gas exchange
- Transcutaneous monitoring allows continuous measurement (TcCO2 and TcO2)
- Use this guideline to set up and safely use transcutaneous monitoring equipment
Clinical indications
- Monitoring adequacy of arterial oxygenation and/or ventilation
- Nursing critically ill or unstable baby
Advantages
- Reduction in number of blood gas measurements
- Immediate recognition of need for ventilation adjustment
Potential problems
- Tissue injury (e.g. erythema, blisters, burns, and skin tears) as a result of failure to change site frequently enough (2–3 hrly)
- Inadequate measurement resulting from incorrect set-up
EQUIPMENT
- Transducer: insert at end position of rack for easy accessibility
- Membranes
- Electrolyte solution
- Adhesive fixation rings
- Recalibration machine
Probe placement and application of fixation rings
- Avoid bony surfaces: use soft tissues (e.g. abdomen, buttock, thigh) and avoid placing over liver as this can prevent accurate clinical assessment of liver size
- Ensure chosen site is clean and dry
- Peel adhesive protection layer off ring
- Place ring on chosen site pressing gently on centre of ring before running finger around outside. Ensure effective seal as this will affect accuracy of measurement
- Place 3 drops of contact fluid in centre of ring
- Remove transducer from module into ring and turn 1-quarter clockwise to secure
CARE AND MONITORING
Temperature setting
- Keep transducer setting at 44°C for all babies. There is good correlation of TcO2 with heat settings of 44°C, but lower settings will result with under-reading of TcO2 and difference is larger with increasing TcO2
Alarm settings
PPHN
- Exact limits will depend on specific pathology but, for guidance, in term babies with PPHN:
- TcO2 upper 10.0 lower 5.5
- TcCO2 upper 7.0 lower 5.0
Blood gas sampling
- Take blood gas 20 min after commencing transcutaneous monitoring to allow comparison between transcutaneous values and arterial partial pressures of O2 and CO2 levels, as discrepancy can occur
- If transcutaneous monitoring values change suddenly, check contact is in place before making ventilator changes. If any doubt about accuracy of values, check blood gas before making ventilator changes
Changing measurement site
- Babies <29 weeks: change 2-hrly
- Babies ≥29 weeks: change 3-hrly
- Unscrew transducer before removing fixation rings
- Remove fixation rings when repositioning baby from supine to prone and vice-versa to avoid pressure sore from lying on rings
- Remove rings 12-hrly on babies <29 weeks and 24-hrly on babies ≥29 weeks
Calibration of membrane
- See Figure 1–5
Indications
- Transducer membrane has been replaced
- Monitor displays 'calibration required'
- Measurement values in doubt
- Applying to a new baby
- Changing measurement site
Ensure calibrator turned off after use. Do not dispose of connecting tube.
Contact technicians when calibrating gas empty
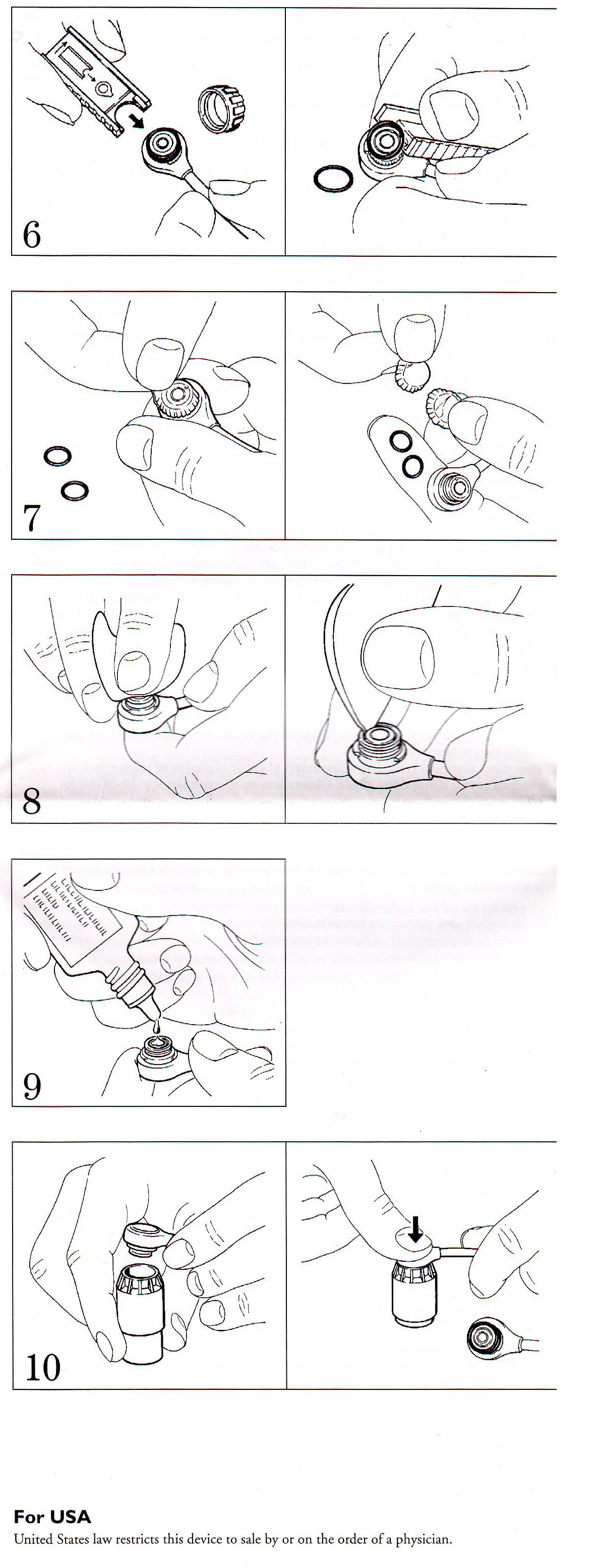
Changing transducer membranes – see Figure 6–10
- All staff responsible for ventilated babies can change transducer membranes
Indications
- When using a new transducer or if transducer has dried out
- For each new baby
- When membrane crinkled, scratched or damaged
- After 5 days continuous use
Procedure
- Wash and dry hands
- To remove O-rings, unscrew protective cap from transducer and hook O-ring remover under them
- Remove both clear plastic membranes with your fingers
- To ensure correct values, clean transducer head, including groove and rim, with absorbent paper to remove all old electrolyte solution
- Apply approximately 2 drops of electrolyte solution to transducer head
- Press transducer head downward into an unused membrane replacer until replacer reacts as far as it can and a click is heard
Figure: 1–5: Calibration of membrane
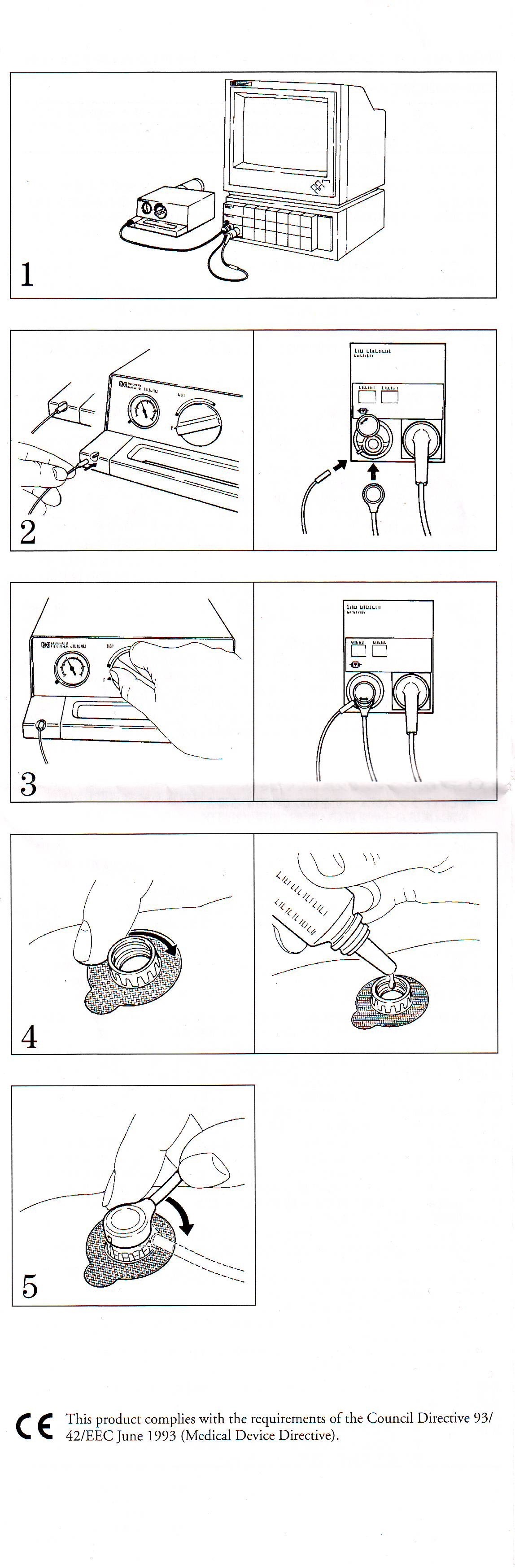
Figure: 6–10 Changing transducer membranes
Date updated: 2024-01-29