Exchange transfusion replaces withdrawn baby blood with an equal volume of donor blood
Discuss all cases with local consultant and arrange urgent transfer to tertiary unit
INDICATIONS
Haemolytic anaemia
- A newborn who has not had an in-utero transfusion (IUT) with a cord Hb <120 g/L and is haemolysing, may require urgent exchange transfusion to remove antibodies and correct anaemia:
- if Hb <100 g/L: discuss urgently with consultant and proceed to exchange transfusion; avoid simple packed cell transfusions
- if Hb 100–120 g/L: obtain 6-hrly bilirubin values and, if rapidly rising or close to exchange transfusion level (see Jaundice guideline), use intravenous immunoglobin (IVIG)
- A newborn who has had IUTs and whose Kleihauer test (may not be available in every hospital) demonstrates a predominance of adult Hb, anaemia can be managed using a top-up transfusion of irradiated, CMV-negative blood
Hyperbilirubinaemia
- Discuss promptly with consultant. If bilirubin values approaching guidance below; senior decision required:
- guidance as determined by exchange transfusion line on gestation-specific NICE jaundice chart (see Jaundice guideline)
- if bilirubin rises faster than 8.5 micromol/L/hr despite phototherapy, anticipate need for exchange transfusion
Other indications
- Chronic feto-maternal transfusion
- Disseminated intravascular coagulation (DIC)
- Severe non-haemolytic anaemia with normovolaemia
COMPLICATIONS
- Cardiac arrhythmias
- Air embolism
- Necrotising enterocolitis
- Coagulopathy
- Apnoeas and bradycardia
- Sepsis
- Electrolyte disturbances
- Acidosis owing to non-fresh blood
- Thrombocytopenia
- Late hyporegenerative anaemia
PROCEDURE
Prepare
- Ensure full intensive care space and equipment available and ready
- Allocate 1 doctor/practitioner and 1 member of nursing staff, both experienced in exchange transfusion, to care for baby during procedure. Document their names in baby’s notes
- Obtain written consent and document in baby’s notes
- Calculate volume of blood to be exchanged: double volume exchange removes 90% of baby’s red cells and 50% of available intravascular bilirubin. Use:
- term babies: 160 mL/kg
- preterm babies: 200 mL/kg
- For anaemia without antibodies or hyperbilirubinaemia use single volume exchange. For term baby use 80 mL/kg, for preterm baby use 100 mL/kg
- Order appropriate volume (usually 2 units) of blood from blood bank, stipulating that it must be:
- crossmatched against mother’s blood group and antibody status, and (if requested by your blood bank) baby’s blood group
- CMV-negative
- irradiated (shelf-life 24 hr) for any baby who has had an in-utero blood transfusion
- as fresh as possible, and certainly ≤4 days old
- plasma reduced red cells for ‛exchange transfusion’ (haematocrit 0.5–0.6), not SAG-M blood and not packed cells
Prepare baby
- Empty stomach using nasogastric tube (see Nasogastric tube insertion guideline) and keep baby nil-by-mouth
- Start IV infusion
- Pay attention to thermoregulation, particularly if procedure to be performed under radiant heater
- Commence continuous cardiac, temperature and saturation monitoring
- If exchange for hyperbilirubinaemia continue phototherapy during exchange transfusion
Document
- Blood pressure, respiratory rate, temperature, SpO2 and heart rate every 15 min throughout exchange
- Volume of blood in and out with each cycle, and keep a running total
If any change in baby’s cardiorespiratory status, pause exchange by priming catheter with donor blood that will not clot. Discuss with consultant
Prepare blood
- Set up blood warmer early (aim for 37°C)
- do not use if:
- intermittent bolus infusion i.e. single catheter exchange
- blood is exposed to a radiant heater (risk of haemolysis)
- do not use if:
- Check blood units as per hospital policy
- Connect donor blood to filter and prime blood giving set
- Connect to 4-way (if using UVC) or 3-way tap (outside the warmer) as indicated
- Gently squeeze donor blood bag before transfusion and every 15 min during, to prevent settling of red blood cells
Technique
- Ensure working area sterile
Either
-
Single catheter push-pull technique
-
sequential withdrawal of baby’s blood and infusion of donor blood via a UVC (see Umbilical venous catheter: insertion and removal guideline)
-
Or
- Isovolumetric or continuous technique
- continuous infusion of donor blood via a venous line with intermittent removal of baby’s blood via an arterial line
use umbilical venous or peripheral venous line for infusion and umbilical arterial or peripheral arterial line for removal of - blood (see Umbilical arterial catheterisation and removal, Umbilical venous catheterisation and removal and Arterial line insertion guidelines)
Single catheter or ‛push-pull’ technique
- Connect catheter bag (using Vygon connector) and donor blood to 4-way tap and 4-way tap to UVC
- Remove 10 mL baby blood from UVC using syringe
- Send first sample (pre-exchange bloods) for serum bilirubin, full blood count, blood culture, blood glucose, calcium, electrolytes, coagulation, liver function tests and bloodspot screening (if not already done)
- when exchange performed for reasons other than known blood group antibodies, send blood for G6PD screening and viral serology
- Replace precise volume removed with donor blood, slowly using a syringe
- Each out-in cycle should replace ≤8.5 mL/kg and take ≥5 min; start with smaller aliquots (10 mL) and increase to 20 mL (if baby stable and weight allows) only after 30 min. As a guide:
- birth weight <1000 g: use 5 mL aliquots
- birth weight 1000–2000 g: use 10 mL aliquots
- birth weight >2000 g: use 20 mL aliquots
- Discard ‛out’ baby blood into catheter bag
- Continue out-in cycles every 5 min (maximum aliquot with each cycle) until complete
- Send last ‛out’ baby blood sample for serum bilirubin, full blood count, blood culture, blood glucose, calcium and electrolytes (post-exchange bloods)
Isovolumetric or continuous technique
- Connect catheter bag, using Vygon connector, to 3-way tap attached to arterial line extension
Never leave arterial line open to catheter bag
- Connect donor blood to venous catheter
- Remove 10 mL of baby’s blood from arterial line and send for tests as listed above under Single catheter or ‛push-pull’ technique
- Start venous infusion at rate to match withdrawal rate e.g. 120 mL/hr for a 10 mL volume withdrawal every 5 min
- Remove ‘out’ aliquots of baby’s blood from arterial line every 5 min to match volume of donor blood being infused into venous line
- Observe limb distal to arterial line at all times and document appearance. If concerned, pause exchange and discuss with consultant
- Continue steps as above but note that continuous ‛in’ cycle requires removal of ‛out’ aliquots only every 5 min
- If exchange stopped for >2–3 min, discontinue procedure and ensure all lines are flushed with sodium chloride 0.9%
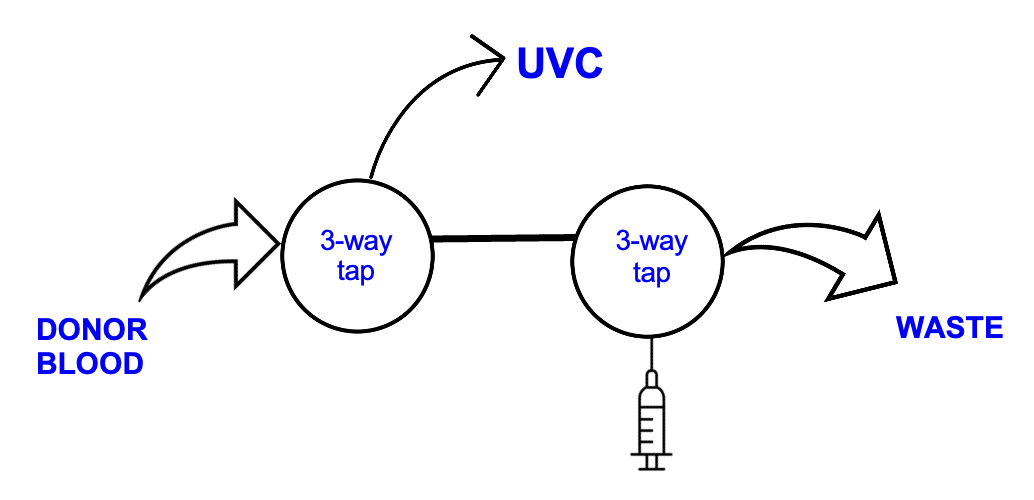
Figure 1: Set-up for single catheter push-pull technique
Immediate
- When Hb and bilirubin in final ‘out’ sample known, check with consultant before removing all lines
- Complete documentation (volumes in/out, and all observations)
- Recommence feeds 4–6 hr after completion
- Monitor blood sugar 4-hrly until acceptable on 2 consecutive occasions (see Hypoglycaemia guideline)
- Update parents
Intermediate
- In babies receiving antibiotics, a repeat dose may be required – discuss with consultant
- Delayed Guthrie spot collection is indicated, as directed by regional centre
Follow-up
- Neurodevelopmental follow-up in all babies who have undergone exchange transfusion
- Repeat full blood count at intervals (likely 1–2 weekly but to be determined individually) for ≥6 weeks, to detect anaemia secondary to ongoing haemolysis
Date updated: 2024-01-16