BABIES <37 WEEKS' GESTATION
Management of these babies should follow the guidance below with the following amendments
- Use blood glucose threshold of >2.6 mmol/L (instead of 2.0 mmol/L)
- Continue to monitor blood sugar pre-feed until 4 consecutive values >2.6 mmol/L
- Screen all babies <37 weeks for hypoglycaemia
- Use nasogastric (NG) feeds (see Nasogastric tube administration of feed, fluid or medication guideline) in preference to IV fluids for a well baby who is unable to take sufficient milk volumes orally
- If baby 34–36+6 weeks unable to tolerate NG feeds, admit to NNU for IV fluids
BABIES ≥37 WEEKS' GESTATION
- Follow the guidance below which is based on Identification and Management of Neonatal Hypoglycaemia in the Full Term Infant – A Framework for Practice, British Association of Perinatal Medicine April 2017
RISK FACTORS FOR HYPOGLYCAEMIA
- Intrauterine growth restriction
- birth ≤2nd centile (Table 1) or
- clinically wasted
- Babies of diabetic mother
- Babies of mother taking beta blockers in third trimester and/or at time of delivery
Table 1: Second centile weights for boys and girls by week of gestation
|
Gestational age |
Weight (kg) | |
| Boys | Girls | |
| 37 | 2.10 | 2.00 |
| 38 | 2.30 | 2.20 |
| 39 | 2.50 | 2.45 |
| 40 | 2.65 | 2.60 |
| 41 | 2.80 | 2.75 |
| 42 | 2.90 | 2.85 |
CLINICAL SIGNS SUGGESTIVE OF HYPOGLYCAEMIA
- Presence of ≥1 of the following clinical signs/diagnoses is an indication to measure blood glucose:
- perinatal acidosis (cord arterial or baby pH <7.1 and base deficit ≥-12)
- hypothermia (<36.5°C) not attributable to environmental factors
- suspected/confirmed early neonatal sepsis
- cyanosis
- apnoea
- altered level of consciousness
- seizures
- hypotonia
- lethargy
- high pitched cry
- Abnormal feeding behaviour (not waking for feeds, not sucking effectively, appearing unsettled, demanding very frequent feeds) especially after a period of feeding well may be indicative of hypoglycaemia
- Jitteriness (excessive repetitive movements of ≥1 limb which are unprovoked and not in response to stimulus) is common and is not by itself an indication to measure blood glucose
MEASUREMENT OF BLOOD GLUCOSE
- Accurate measurement of blood glucose level is essential for diagnosis and management of neonatal hypoglycaemia
- A ward-based blood gas biosensor (blood gas machine) should be considered the reference standard for measuring blood glucose
- All current cot-side devices are prone to inaccuracy, particularly in the range 0–2.0 mmol/L
- If handheld glucometer used:
- confirm low values using an accurate method (blood gas analyser or laboratory sample)
- use only devices conforming to ISO 15197:2013 standard
- Blood samples with high PCV can produce erroneously low results
INITIAL MANAGEMENT OF BABY AT RISK OF HYPOGLYCAEMIA
- Provide parents with written information, e.g. https://hubble-live-assets.s3.amazonaws.com/bapm/attachment/file/53/Identification_and_Management_of_Neonatal_Hypoglycaemia_in_the__full_term_infant_-_A_Framework_for_Practice_revised_Oct_2017.pdf
- Ensure baby kept warm and commence skin-to-skin contact
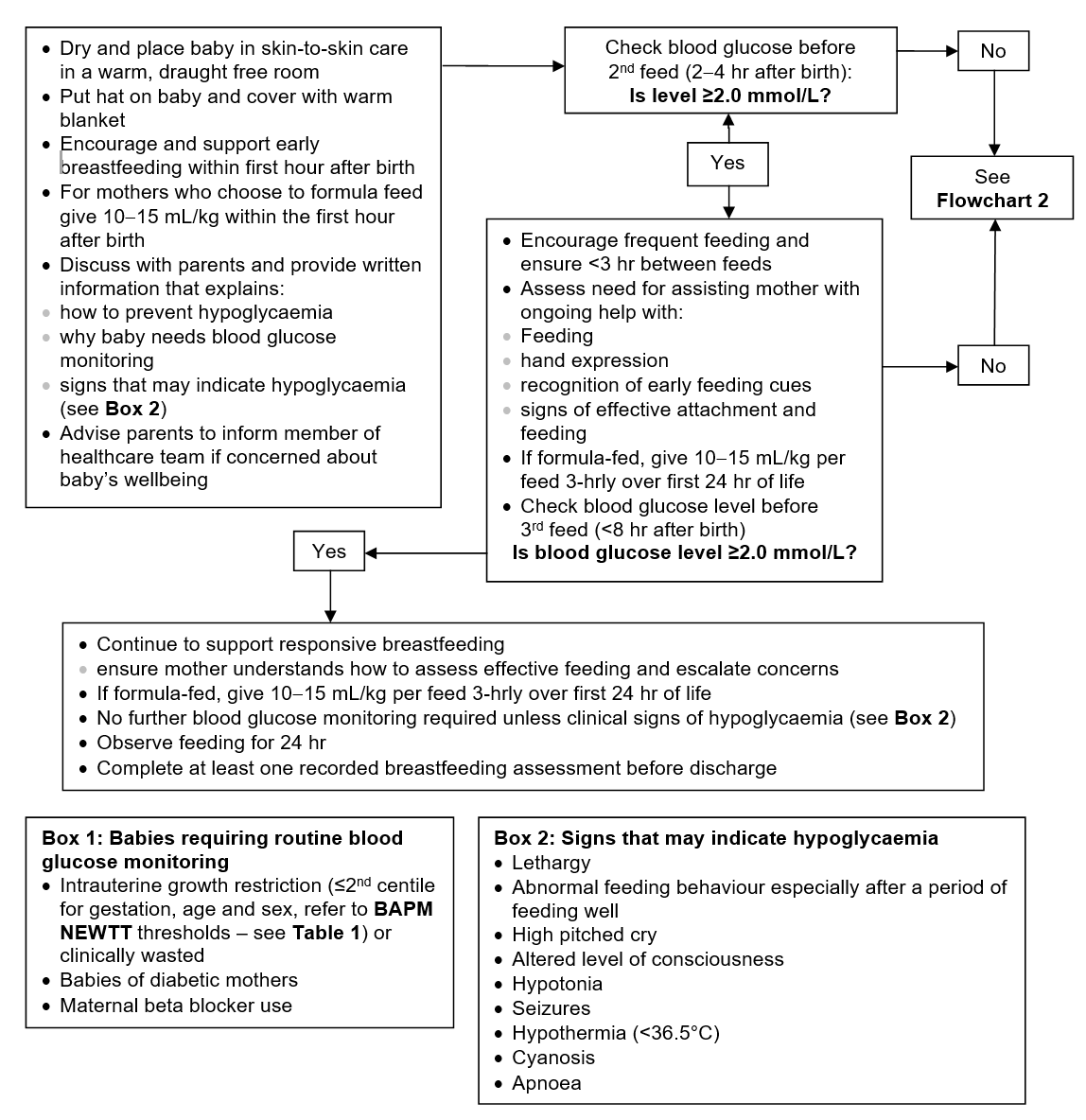
- Begin care pathway in Flowchart 1
- Ensure baby offered feed within first hour
- Offer breast in response to feeding cues as often as possible
- Do not allow >3 hr between feeds until 2 consecutive blood glucose measurements >2.0 mmol/L
- If baby not showing signs of effective feeding:
- encourage continuous skin-to-skin contact and encourage mother to hand express
- continue to express 8–10 times in 24 hr until baby feeding effectively
- if no colostrum available, discuss with mother and supplement with formula milk 10–15 mL/kg until colostrum available
- If mother chooses to formula feed:
- offer 10-15 mL/kg within the first hour and plan to feed 3-hrly
- when 2 consecutive blood glucose measurements >2.0 mmol/L, demand feed
- Measure blood glucose level before second feed (2–4 hr after birth), or sooner if clinical signs suggestive of hypoglycaemia
SUBSEQUENT MANAGEMENT
Based on first blood glucose result, place baby on 1 of the following care pathways:
First pre-feed blood glucose ≥2.0 mmol/L
- Continue to follow Flowchart 1
- Check blood glucose before third feed (≤8 hr after birth)
- if ≥2.0 mmol/L no further blood glucose measurement required. Observe feeding in hospital for 24 hr and complete at least 1 breastfeeding assessment before discharge (see Breastfeeding guideline)
- if <2.0 mmol/L follow Flowchart 2
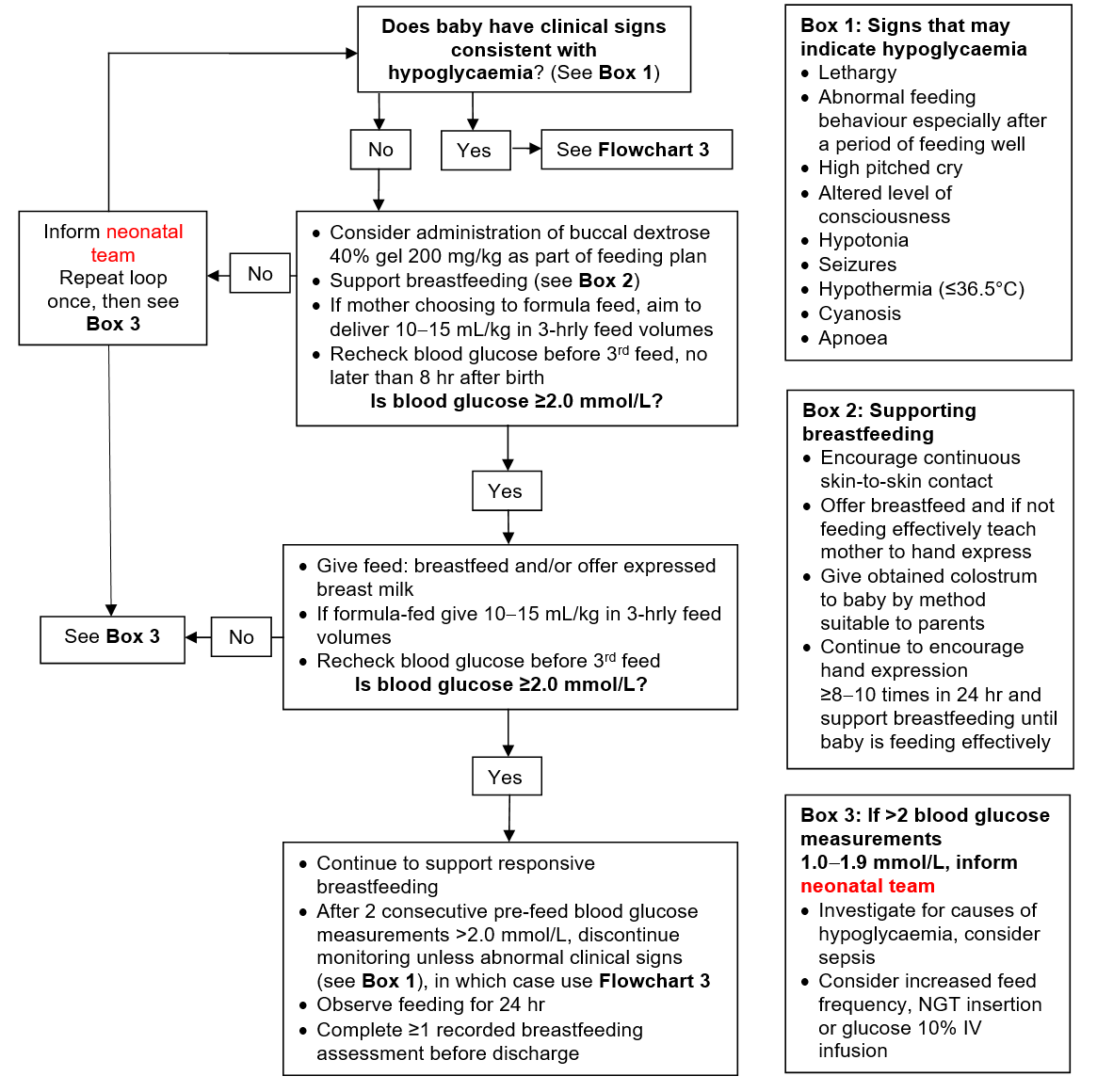
First pre-feed blood glucose 1.0–1.9 mmol/L and no abnormal signs
- Follow Flowchart 2
- Buccal dextrose 40% gel 200 mg/kg (0.5 mL/kg of 40% gel) may be used as part of feeding plan
use 2.5 or 5 mL oral/enteral syringe- dry oral mucosa with gauze, gently squirt gel with syringe (no needle) onto inner cheek and massage gel into mucosa using latex-free gloves
- offer a feed (preferably breast milk) immediately
- repeat blood glucose measurement as requested
- if baby remains hypoglycaemic repeat buccal dextrose 40% gel (see Flowchart 2)
- maximum 6 doses in 48 hr
- discuss with neonatal team before giving second dose
- examine baby before third dose
- Continue to support feeding as above
- After 2 consecutive values >2.0 mmol/L discontinue blood glucose measurement. Observe feeding for 24 hr and complete ≥1 breastfeeding assessment before discharge (see Breastfeeding guideline)
- If baby displays clinical signs consistent with hypoglycaemia, or >2 measurements 1.0-1.9 mmol/L, follow Flowchart 3
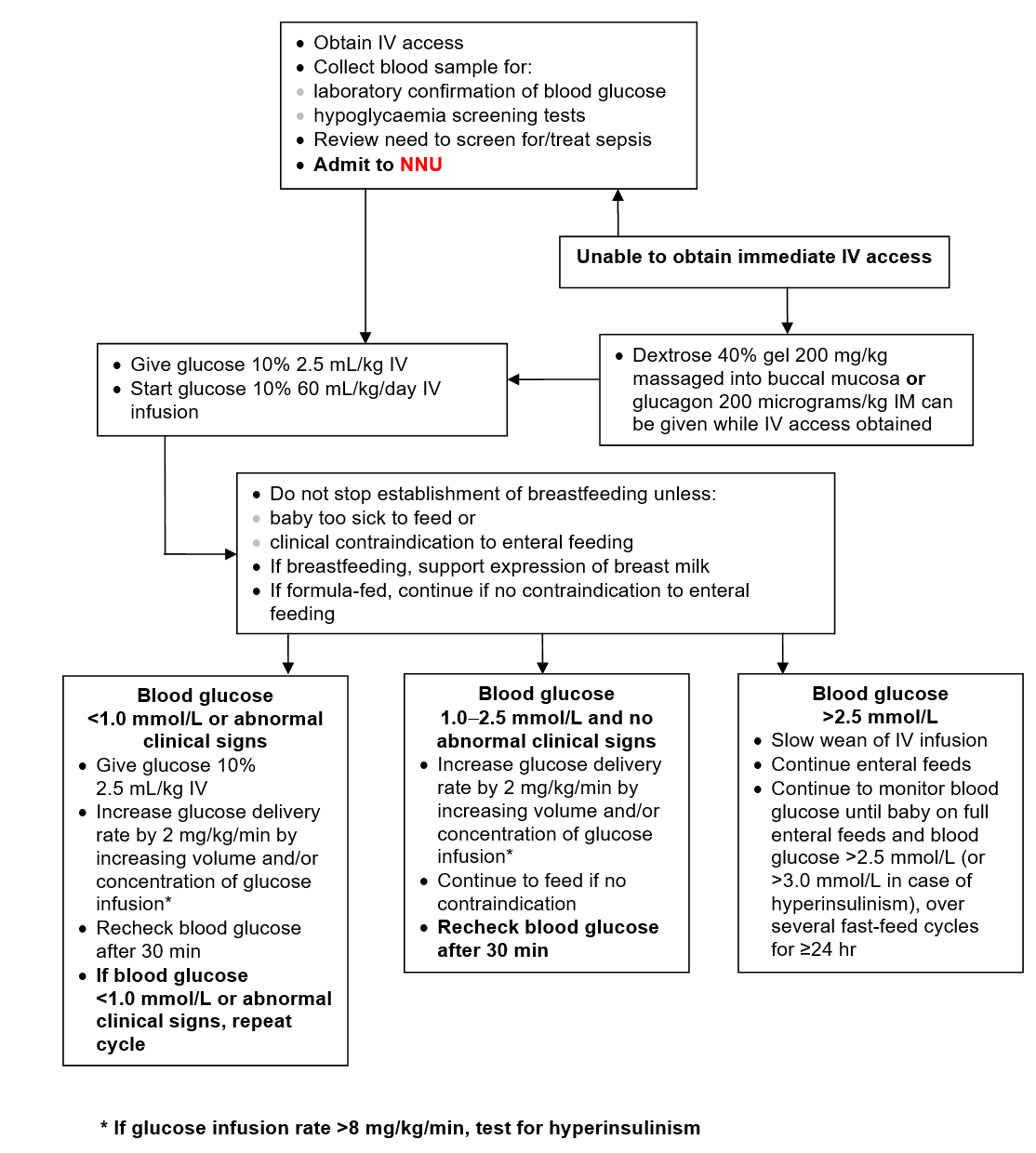
First pre-feed blood glucose <1.0 mmol/L, and/or clinical signs consistent with hypoglycaemia
- Follow Flowchart 3
- Seek urgent medical attention and admit to NNU
- Obtain IV access
- Collect blood samples for confirmation of blood glucose and hypoglycaemia screening tests (see Investigations)
- Review need to screen for/treat sepsis (see Infection in the first 72 hours of life guideline)
- Give glucose 10% 2.5 mL/kg IV and start infusion of glucose 10% at 60 mL/kg/day
- If unable to obtain immediate IV access, as an interim measure whilst awaiting IV access, give either:
- buccal dextrose 40% gel 200 mg/kg (equivalent to 0.5 mL/kg of 40% gel) as detailed above or
- single dose of glucagon 200 microgram/kg IM
- Recheck blood glucose after 30 min and continue to follow Flowchart 3
INVESTIGATIONS FOR HYPOGLYCAEMIA
Indications
- Persistent hypoglycaemia (>2 measurements <2.0 mmol/L within the first 48 hr of life)
- Severe hypoglycaemia (<1.0 mmol/L) at any time
- Signs of acute neurological dysfunction and blood glucose <2.5 mmol/L at any time
Investigations
Perform following investigations during the period of hypoglycaemia
- Blood
- glucose
- insulin
- cortisol
- growth hormone
- fatty acids
- ketone bodies
- carnitine
- acylcarnitine profile
- amino acids
- ammonia
- lactate
- Urine
- ketones
- organic acids
- Review need to screen for/treat sepsis (see Infection in the first 72 hours of life guideline)
- Further investigations based on results of initial screen and following specialist advice
- Transient hypoglycaemia, defined as 1 measurement 1.0-1.9 mmol/L within the first 48 hr of life, in baby with no abnormal signs who is feeding effectively, does not require investigation
PERSISTENTLY LOW BLOOD GLUCOSE MEASUREMENT
- Defined as >2 measurements <2.0 mmol/L within the first 48 hr of life
- May be the first sign of hyperinsulinism or another metabolic disorder characterised by hypoglycaemia
- If blood glucose concentration remains low (<2.0 mmol/L) on ≥3 occasions in the first 48 hr, despite adequate energy provision and a feeding plan, or a glucose dose >8 mg/kg/min (glucose 10% 115 mL/kg/day infusion) is required, suspect hyperinsulinism
- Babies with suspected or confirmed hyperinsulinism may require non-standard glucose infusions to achieve target blood glucose concentration. See below for advice on making up such an infusion
- If hyperinsulism suspected or confirmed, aim to maintain blood glucose >3.0 mmol/L until insulin levels are known
- Hyperinsulinism confirmed if paired insulin and glucose measurements taken whilst hypoglycaemic give glucose:insulin ratio <0.3, or if insulin >10 picomole/L when glucose <2.0 mmol/L
- If baby suspected of having hyperinsulinism discuss with the national centre for hyperinsulinism at Royal Manchester Children’s Hospital
- Give glucose >12.5% infusion via a central line [see Umbilical venous catheter insertion and removal and Long line insertion (peripherally sited) guidelines]
Calculation of glucose infusion rate
Glucose infusion rate in mg/kg/min = % glucose x fluid volume in mL/kg/day / 144
IV glucose concentration
|
Flow rate of glucose 10% |
Infusion rate |
| 40 | 2.77 |
| 60 | 4.16 |
| 80 | 5.55 |
| 100 | 6.94 |
| 120 | 8.33 |
| 130 | 9.03 |
| 140 | 9.72 |
| 150 | 10.42 |
To make up any concentration of glucose in any volume
- Desired volume = V mL
- Desired concentration of glucose = D%
- Lower concentration of glucose = L%
- Volume of lower concentration of glucose to add = LV mL
- Higher concentration of glucose = H%
- Volume of higher concentration of glucose to add = HV mL
| Formula |
HV = V (D−L) / (H−L) LV = V−HV |
| HV mL + LV mL = V mL of D% |
If >12.5% glucose required, give via a central line [see Umbilical venous catheter insertion and removal and Long line insertion (peripherally sited) guidelines]
FLOWCHARTS
Flowchart 1: Management of babies ≥37 weeks at risk of hypoglycaemia
Flowchart 2: Pre-feed blood glucose 1.0-1.9 mmol/L and no abnormal clinical signs
Flowchart 3: Blood glucose <1.0 mmol/L and/or clinical signs consistent with hypoglycaemia
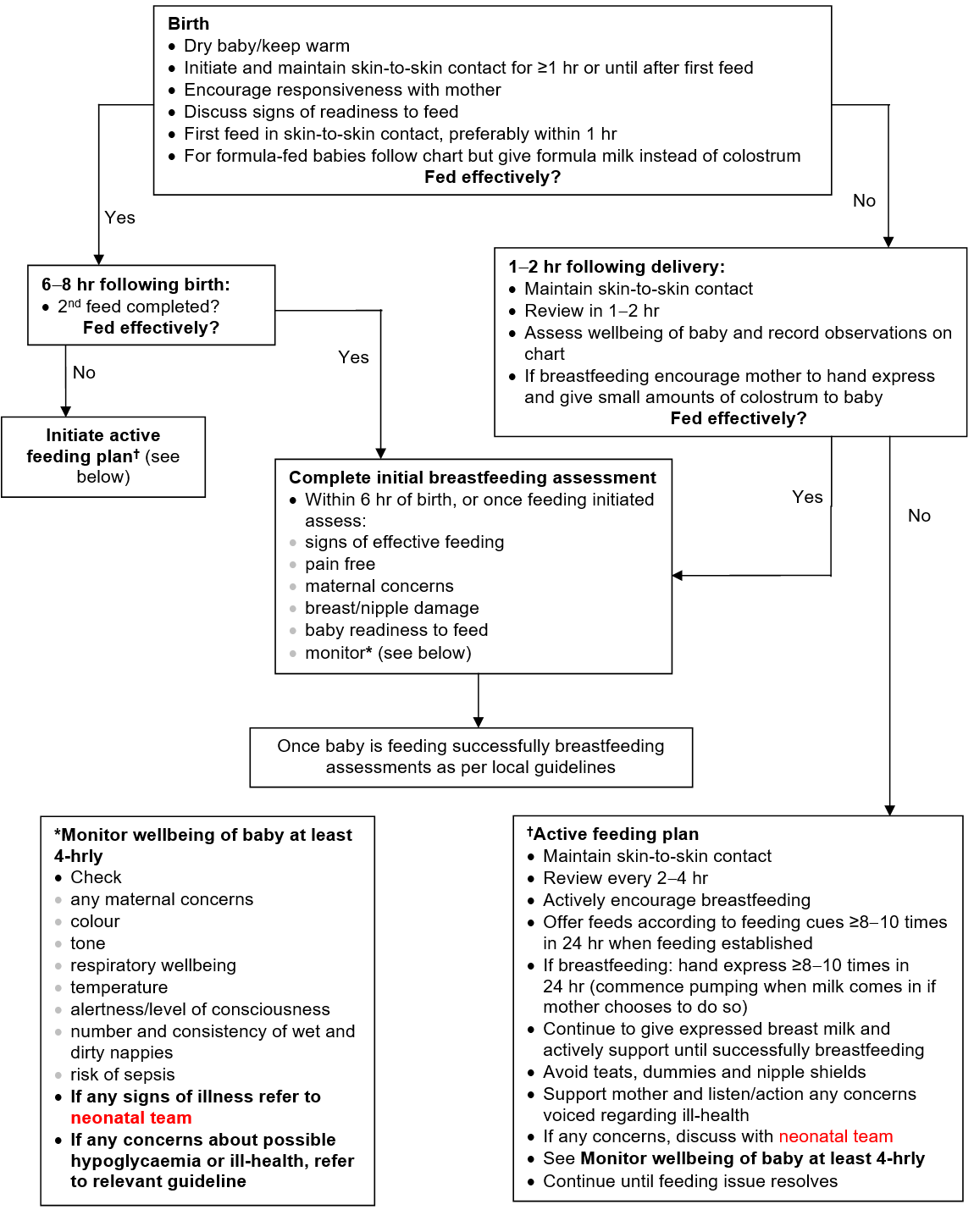
Flowchart 4: Management of reluctant feeding in healthy breastfed babies ≥37 weeks
Date updated: 2024-01-11