BACKGROUND
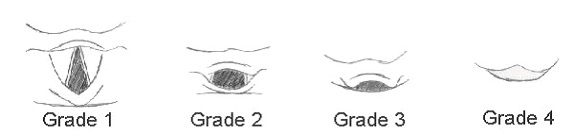
In most babies, direct laryngoscopy results in a clear view of the larynx. The laryngeal view is classified by Cormack and Lehane as follows:
|
Grade 1 |
Visualisation of entire laryngeal aperture There should be no difficulty in intubation |
|
Grade 2 |
Visualisation of just the posterior portion of laryngeal aperture May be slight difficulty Cricoid pressure should improve visualisation |
|
Grade 3 |
Visualisation of only the epiglottis Can result in severe difficulty; cricoid pressure may be helpful |
|
Grade 4 |
Visualisation of soft palate only, not even the epiglottis is visible Always difficult and usually accompanies obvious pathology but may also occur totally unexpectedly. Senior support may be required |
difficulty with face mask ventilation and/or tracheal intubation
MANAGEMENT PLAN
- Use premedication as appropriate for your unit
- Good practice to have team around the baby familiar with each other’s names, and assigned roles for the intubation (e.g. team leader with oversight, medication, equipment)
- Difficult neonatal intubation may occur at or after delivery and may be:
- anticipated (e.g. Pierre Robin sequence, Treacher–Collins, cleft lip and palate, Goldenhar syndrome, Apert/Crouzon syndrome, Down’s syndrome) or
- unanticipated (e.g. subglottic stenosis, laryngeal atresia, laryngeal or tracheal webs, glottic oedema post extubation)
- Where difficult intubation is anticipated, ensure senior help is available before commencing (senior experienced middle grade, consultant or, if indicated, ENT consultant/anaesthetist)
Difficult airway pack
- Infant oropharyngeal airways (Guedel, sizes 000, 00, 0)
- ETT size 2–4.5 with stylet for intubation
- ETT size 2–4.5 with scissors, to cut short for use as nasopharyngeal airway support
- ETT fixation equipment
- Straight bladed laryngoscopes for big and small baby
- Forceps
- Supraglottic airway devices, e.g. laryngeal mask airways (LMAs) with inflatable cuff size 1 for babies >2 kg or i-gel with non-inflatable cuff size 1 for babies 2–5 kg
- Size 2.5–4.5 endotracheal bougies for railroading ETT
- Video laryngoscope and blades if available on your unit
- CO2 detector e.g. Pedicap®
Can ventilate, cannot intubate
(Good chest excursion and rising/good heart rate but baby still needs intubation)
-
No more than 4 attempts at intubation (2 per individual resuscitator), to avoid laryngeal oedema and convert this into a ‘cannot intubate, cannot ventilate’ scenario
-
ventilate between attempts at intubation
-
maximum 30 sec per attempt to limit hypoxia
-
-
Call for senior help
-
If intubation attempts fail, stop. Continue either bag and mask ventilation or LMA ventilation until senior help available
-
it is safer to maintain ventilation with mask ventilation with adequate chest expansion until help arrives, as baby is less likely to tolerate repeated unsuccessful ETT attempts
-
-
2 further attempts by senior trainee/neonatologist
-
Try indirect laryngoscopy using video laryngoscope if available. If this fails, call for ENT support for rigid bronchoscopy or surgical tracheostomy, or ENT/anaesthetist for flexible fibrescope assisted intubation depending on your hospital’s availability
-
Use end tidal CO2 detectors (e.g. Pedicap®) to confirm tracheal intubation
Cannot ventilate, cannot intubate
-
Call for senior help
-
Reconfirm the following:
-
neutral head position (overextension can limit vision)
-
correct size face mask being used, create a tight seal
-
use correct size oropharyngeal airway (Guedel airway): too big may cause laryngospasm and too small may worsen obstruction. (Tip of Guedel airway should reach angle of jaw when aligned with lip on side of face)
-
use 2 person jaw-thrust
-
ensure pressures for mask ventilation are adequate
-
cold light to exclude pneumothorax
-
-
For specific conditions (e.g. Pierre Robin sequence, micrognathia) nasopharyngeal airway may be useful. To make, take an ETT and shorten it by measuring distance between nasal tip and ear tragus. Choose a size that does not blanch the nares completely when inserted
-
Ventilation with supraglottic airway devices (LMA with inflatable cuff size 1 for babies ≥2 kg or i-gel with non-inflatable cuff size 1 for babies 2–5 kg)
-
When senior help arrives:
-
reattempt intubation
-
use a small towel roll under baby’s shoulder to improve vision
-
use indirect laryngoscopy with video laryngoscope if available
-
-
Call ENT or anaesthetist for support (ENT for rigid bronchoscopy or surgical tracheostomy, or anaesthetist for flexible fibrescope assisted intubation as above, depending on your hospital’s availability)
-
Use end tidal CO2 detector (e.g. Pedicap®) to confirm tracheal intubation
Prevent/anticipate difficult intubation/reintubation
- For ventilated babies due for extubation, risk of difficult reintubation can be reduced by pre-extubation dexamethasone to reduce cord oedema, especially in babies who had difficult initial intubations or chronic ventilatory course
- if ETT leak <10–15%, consider dexamethasone
Common problems with intubation
|
Problem |
Action |
|
Oesophageal intubation – blade placed too deep, cords not visualised |
|
|
Tongue obscures vision |
|
|
Cannot see cords |
|
|
Cannot intubate |
|
Seek senior support in the following situations:
- Blind intubation: in small baby where poor visualisation due to size
- Supraglottic airway devices (LMA size 1 or i-gel size 1): can be inserted by juniors while awaiting senior support if trained (see below for details)
- Video laryngoscope: if available, to guide intubation through the cords
- Railroad technique: if laryngeal aperture narrow, insertion of stylet through cords, and railroading ETT over it
- usually a 2-person procedure and can be carried out under direct vision/blind, depending on visual field and equipment
- carefully insert a bougie through vocal cords, ≤2 cm beyond aperture opening
- keep bougie steady while colleague threads ETT over top end of stylet and into trachea. Note: using a stylet from the ETT pack carries risk of oesophageal/tracheal perforation
- Ultra-small fibre-optic bronchoscopy (if available locally): with railroading via bronchoscope
- Surgical tracheostomy: not undertaken by neonatal consultants – seek ENT support
- Note: Prolonged procedure - additional dose of muscle relaxant can be used under senior guidance
- ensure venous access obtained
- support cardiac system with IV fluid boluses as required
- use inotropic agents as required, based on perfusion and blood pressure (see Hypotension guideline)
- Keep baby warm using techniques supported by your local unit e.g. TransWarmer®, bubble wrap
- Empty stomach contents regularly while on face mask/T-piece ventilation
I-GEL
- Supraglottic mask with soft non-inflatable cuff attached to an airway tube
- Once inserted anterior tip enters upper oesophagus while cuff conforms to contours of perilaryngeal structures, with lumen facing laryngeal opening
- Once successfully inserted can be connected to a positive pressure inflation device i.e. ambu bag/Neopuff™
- Size 1 suitable for babies >2 kg, usually ≥34 weeks’ gestation
- ETT can be passed (size 3) through central port within i-gel (size 1)
Indications
- Babies >2 kg, ≥34 weeks’ gestation when:
- bag and mask ventilation ineffective/problematic and endotracheal intubation unsuccessful
- bag and mask and endotracheal intubation not immediately feasible due to facial and/or airway deformities
- may be beneficial as a more stable airway during transport of sick neonate (needing positive pressure ventilation by mask) by paramedics/midwifery staff from home or midwifery-led unit to NNU
i-gel should not be used:
- In the setting of meconium-stained amniotic fluid
- When chest compressions required
- For delivery of drugs into the trachea
Advantages
- Ease of insertion
- Minimal risk of tissue compression and instability after insertion
- Easily learned skill and easily replicated
- Less invasive than endotracheal intubation
- Insertion does not require neuromuscular blockers and sedation
Insertion technique
- Place head centrally in ‘air-sniffing’ position
- Remove i-gel from sterile protective cage
- Grasp i-gel close to the connector; lubricate back, sides and front of cuff with a thin layer of lubricating gel, ensuring no lubricant remains in the bowl of the cuff (oral secretions alone may be sufficient to aid movement)
- Depress baby’s chin, thereby enlarging oral cavity
- Grasp i-gel close to cuff, holding it like a pen
- Point i-gel tip cranially against hard palate
- Glide device downwards and backwards along the hard palate with a continuous but gentle push until definitive resistance felt
- i-gel will advance along the posterior pharyngeal wall, with tip locating itself in the upper oesophagus
- Attach to Neopuff™/bag and mask ventilation at pre-set pressures
- Observe for signs of clinical improvement, confirmed by chest movement, increasing heart rate, improving colour and saturations
- Listen for air leaks (may not be in correct position)
- Ensure device remains centrally placed (black i-gel logo visible in central position)
- Once position confirmed and clinically effective, tape from maxilla to maxilla to avoid loss of airway
Following i-gel insertion
- Do not allow peak pressure of ventilation to exceed 40 cm H2O
- Do not use excessive force to insert device
- Excessive air leak during manual ventilation is due to suboptimal depth of i-gel insertion, malposition or excessive peak pressure use
- Do not leave device in situ for >4 hr without senior advice
- Do not reuse the i-gel
- No more than 3 attempts should be attempted in one patient
Complications/side effects
- Malposition
- Vagal response
- Gastric ventilation, distension and aspiration
- Laryngospasm or trauma to the pharyngolaryngeal framework
COMMUNICATION
- Inform parents of procedure and events