Hypovolaemia is an uncommon cause of hypotension in the preterm newborn.
Excessive volume expansion can increase mortality
Excessive volume expansion can increase mortality
DEFINITION
Thresholds for intervention
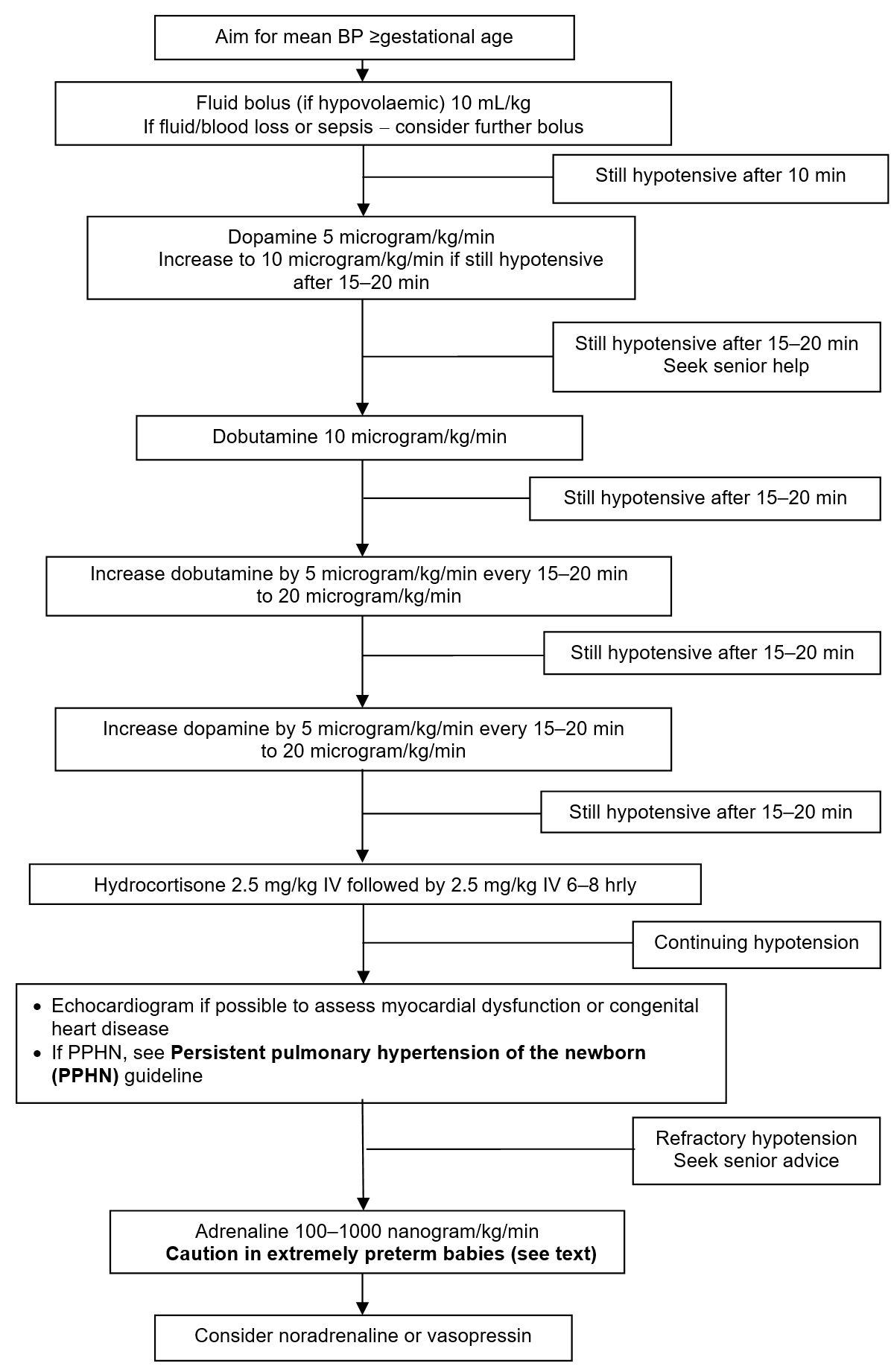
- Aim to maintain mean arterial BP (MABP) ≥ gestational age in weeks
- Aim for even higher MABP in case of persistent pulmonary hypertension of the newborn [see Persistent pulmonary hypertension of the newborn (PPHN) guideline]
RECOGNITION AND ASSESSMENT
Assessment of cardiovascular status
- Measure BP:
- by direct intra-arterial BP [umbilical arterial catheter (see Umbilical artery catheterisation and removal guideline) or peripheral arterial line (see Arterial line insertion) guideline]
- automated oscillometry (Dinamap) has limited accuracy in hypotensive preterm babies; usually over-reads BP in the lower ranges
- Assess tissue perfusion using as many of the following indices as possible (thresholds for abnormality in brackets):
- capillary refill time (>3 sec)
- toe-core temperature difference (>2°C)
- urine output (<1 mL/kg/hr)
- rising lactate
Causes of hypotension
- Sepsis
- Extreme prematurity
- Tension pneumothorax
- Blood loss
- Large patent ductus arteriosus (PDA) (see Patent ductus arteriosus guideline)
- Poor myocardial contractility (very-low-birth-weight, hypoxia, cardiomyopathy or hypocalcaemia)
- Polyuria secondary to glucosuria
- Third spacing (surgical causes – NEC/perforation/malrotation/obstruction)
- High positive intrathoracic pressure (high MAP on conventional/HFOV)
- Severe acidosis (pH <7)
- Drugs (morphine, muscle relaxants and anti-hypertensives)
IMMEDIATE TREATMENT
Aim is to treat cause and improve organ perfusion, not to correct a ‘BP reading’
Seek senior advice throughout
Seek senior advice throughout
Transilluminate chest to exclude pneumothorax (see Transillumination of the chest guideline)
Fluid
- Give if hypovolaemic (not >10 mL/kg) unless evidence of fluid/blood loss/sepsis (late onset sepsis/term babies), when it may be necessary to give more than this volume, depending on condition of baby. Otherwise, start inotropes first (see Inotropes)
- If clinical condition poor, BP very low, or mother has been treated with IV anti-hypertensive agent, give inotrope after fluid bolus
Which fluid?
- Use sodium chloride 0.9% 10 mL/kg over 10–15 min except when there is:
- coagulopathy with bruising: give fresh frozen plasma 10 mL/kg over 30 min (see Coagulopathy guideline)
- acute blood loss: give packed cells 10 mL/kg over 30 min
Reassess clinically within 10 min of bolus
-
If hypotension persists, start inotropes – seek senior advice
Inotropes
Evidence for the best choice of inotropes is lacking and thus this guideline is suggested from the best possible evidence and the safety of the commonly used inotropes
-
Start dopamine at 5 microgram/kg/min
-
Reassess every 15–20 min
-
If still hypotensive, increase dopamine to 10 microgram/kg/min
-
if still hypotensive, add dobutamine at 10 microgram/kg/min
-
if still hypotensive, increase dobutamine up to 20 microgram/kg/min
-
if still hypotensive, increase dopamine up to 20 microgram/kg/min
-
give hydrocortisone 2.5 mg/kg IV (over 3–4 min) followed by 2.5 mg/kg IV 6–8 hrly for 2–3 days as necessary
-
Do not use >20 microgram/kg/min of dopamine (alpha effect causes vasoconstriction)
- In babies with poor cardiac function, consider starting dobutamine first
- In term babies requiring inotropes for pulmonary hypertension an infusion of noradrenaline or adrenaline may be required [see Persistent pulmonary hypertension of the newborn (PPHN) guideline]
- consider milrinone in PPHN after evaluation of cardiac function and discussion with cardiologist
Caution: see BNFc for further information on use and side effects of inotropes (sympathomimetics) and use alternate drugs in presence of excessive tachycardia or other side effects
How
- Inotropes ideally given via central line
- When peripheral line used during emergency (see BNFc for dilutions), monitor site carefully for extravasation injury (see Extravasation injuries guideline)
Continuing hypotension
- Echocardiogram where possible to assess myocardial dysfunction/congenital heart disease
Refractory hypotension
Seek senior advice before starting adrenaline infusion. Depending on individual circumstances, discuss alternative agents (e.g. noradrenaline, vasopressin)
If acidotic with severe hypotension, but not hypovolaemic
- Give adrenaline 100–1000 nanogram/kg/min (see BNFc for instructions on making up solution). If baby requires >1 microgram/kg/min (= >1000 nanogram/kg/min), consider other inotropes
- Monitor limb perfusion and urine output
If cooling for hypoxic ischaemic encephalopathy (HIE) – refer to Hypoxic ischaemic encephalopathy (HIE) including preparation for active cooling guideline. Vasoconstrictive agents can reduce peripheral perfusion
MONITORING
- BP via arterial line (peripheral or UAC) (see Umbilical artery catheterisation and removal or Arterial line insertion guidelines)
- Check effective delivery of drugs:
- record volume in syringe hourly
- check for leaks
- ensure correct position of UVC or long line delivering inotropes
- Chest X-ray:
- if intubated
- urgent, if respiratory status worsening
- look for air leak or over-inflation
- Signs of tissue perfusion:
- blood gases including lactate
- urine output
- capillary refill
- heart rate
- Echocardiogram where possible to assess function and structure
SUBSEQUENT MANAGEMENT
- If already on morphine and muscle relaxant infusion, reduce dosage if possible
- In ventilated babies, especially those on HFOV reduce mean airway pressure cautiously without compromising chest inflation and oxygenation
- If baby acidotic and not responding to treatment, consider sodium bicarbonate
Weaning inotropes if hypotension improves
- Wean inotropes (dopamine or dobutamine) in 5 microgram/kg/min decrements and adrenaline in 100 nanogram/kg/min decrements) as tolerated and directed by senior advice
Flowchart: Management of hypotension [If PPHN, see Persistent pulmonary hypertension of the newborn (PPHN) guideline]
Date updated: 2024-01-08