PRINCIPLES
- Maternal breast milk (MBM) is the optimal feed for all babies. Mothers should be counselled and supported to express milk as soon as possible after birth and frequently thereafter to ensure adequate supply for baby
- Compared to formula milk maternal colostrum and breast milk reduce rates of mortality, BPD and ROP, reduce risks of NEC and sepsis and improves neurodevelopmental outcomes
- Early enteral feeds promote normal gastrointestinal structure and function, motility and enzymatic activity
- Delayed nutrition can result in growth restriction with long-term complications of parenteral nutrition, dysbiosis of the intestine, poor organ growth and poorer neurological outcomes
- Manage feeding on an individual basis dependent upon gastrointestinal tolerance and availability of maternal breast milk
- This guideline is designed to be used in conjunction with individual clinical assessment processes
NUTRITIONAL REQUIREMENTS
Table 1: Daily recommended intake of nutrients for stable growing term and preterm babies
|
Nutrient |
Term baby |
Preterm baby (ESPGHAN 2022) |
|
Energy (kcal/kg/day) |
95–115 |
115–140 (160*) |
|
Protein (g/kg/day) |
2 |
3.5–4.0 (4.5*) |
|
Sodium (mmol/kg/day) |
1.5 |
3.0–5.0 (8.0*) |
|
Potassium (mmol/kg/day) |
3.4 |
2.3−4.6 |
|
Calcium (mmol/kg/day) |
3.8 |
3.0–5.0 |
|
Phosphorous (mmol/kg/day) |
2.1 |
2.2−3.7 |
|
Zinc (mg/kg/day) |
4.0 (mg/day) |
2.0−3.0 |
|
Iron (mg/kg/day) |
1.7 (mg/day) |
2.0−3.0 (6.0*) |
|
Folic acid (µg/kg/day) |
50 (µg /day) |
23−100 |
|
Vitamin A (µg RE/kg) |
59 |
400–1000 |
|
Vitamin D (units/day) |
400 |
400−700 (<1000*) |
*upper intakes that may occasionally be required in routine clinical practice under certain conditions – seek advice from neonatal dietitian
FEEDING GUIDE
- Commence enteral feeds in preterm and sick babies as close to birth as possible (unless clinically contraindicated)
Buccal colostrum
- Provides benefits of colostrum to all sick and preterm babies unable to breast feed orally
- Give to all babies admitted to NNU who are not receiving oral feeds unless maternal breast milk is contraindicated (see Breastfeeding guideline)
- Place 0.3 mL (0.15 mL per side) colostrum in buccal cavity by syringe/gloved finger at 3-hrly intervals for first 48 hr of life
- Parental involvement in administration recommended. Nursing staff may teach and supervise parents to give colostrum
ENTERAL FEEDS
Route of administration
- Most babies <34 weeks are unable to co-ordinate sucking, swallowing and breathing to feed effectively and so should be fed via a naso- or orogastric tube
- Some babies <34 weeks may show feeding cues, especially while in skin-to-skin. They may be offered the breast, but bottle feeds should not be offered until >34 weeks (see Progression to oral feeding in preterm babies guideline)
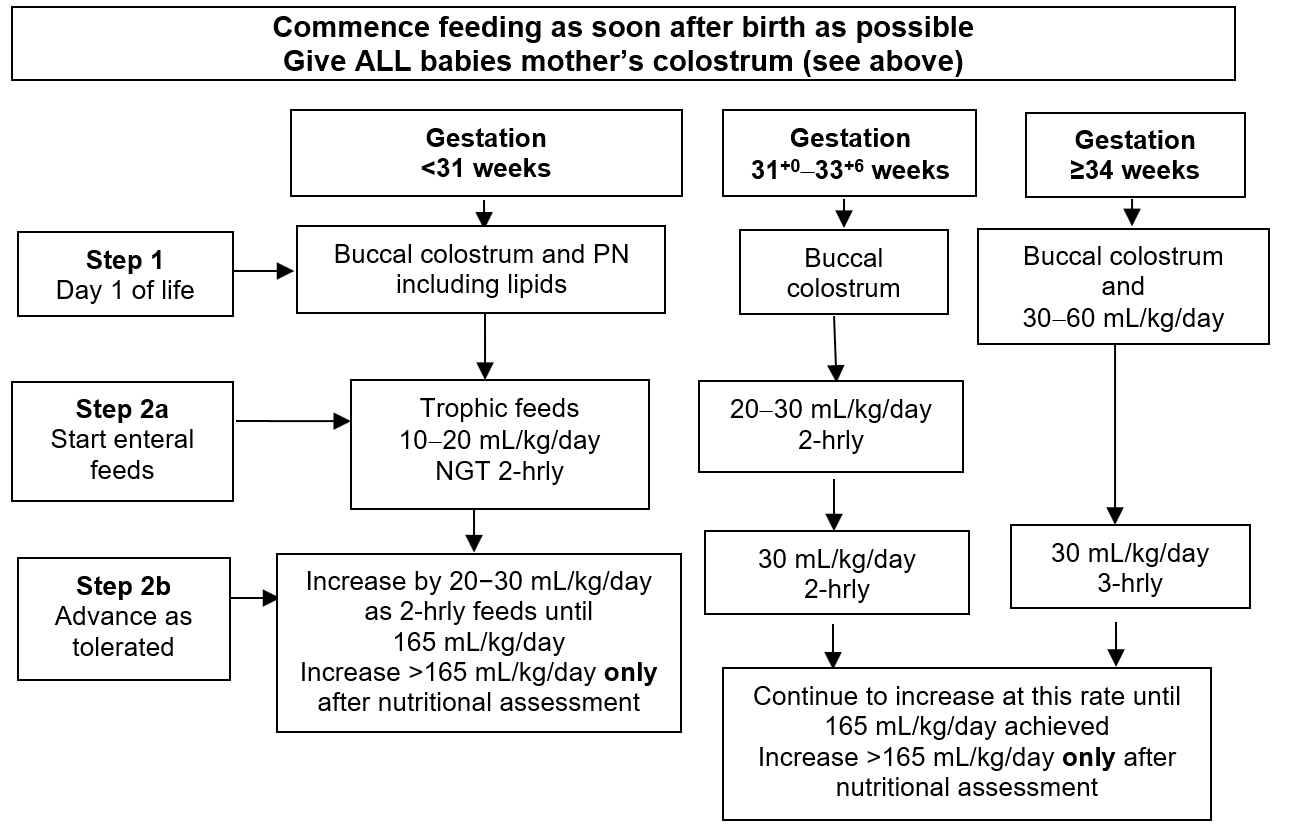
Flowchart 1: Initiating and advancing enteral feeds
Make every effort to use mother’s fresh expressed colostrum and breast milk
Give ALL babies mother’s colostrum (see above)
- If maternal expressed breast milk (MBM) not available within 48 hr of birth, use donor breast milk (DBM), if criteria met, or preterm formula
- If unable to advance enteral feeds in first 3−7days:
- maintain trophic feeds small volumes (10–20 mL/kg/day) intended to stimulate gut trophic hormones
- contact neonatal dietician
- In babies >31+0 review need for parenteral nutrition (see Parenteral nutrition guideline)
PROBIOTICS
- Reduce rates of NEC, sepsis, and mortality in babies born <32 weeks’ gestation
- Insufficient evidence currently to recommend one product over another
- Give to all babies born <32 weeks’ gestation when receiving 20 mL/kg/day enteral feeds
- if baby has stoma, when receiving 50 mL/kg/day enteral feeds
- If enteral feeds stopped, discontinue and restart when baby receiving enteral feeds 20 mL/kg/day
- if baby has stoma, when receiving 50 mL/kg/day enteral feeds
- Stop when baby reaches 34 weeks’ CGA
- Provide parents with WMNODN leaflet on potential benefits and risks of probiotic administration
WHICH MILK TO USE
Maternal breast milk (MBM)
-
Remains the ideal milk for term and preterm babies
-
Support mothers to initiate and maintain expressing (see Breastfeeding guideline)
-
Wherever possible, use MBM for initiation of enteral feeds. If milk supply insufficient for requirements it may not always
be possible to follow feeding schedules until sufficient breast milk is available-
record absence of MBM as ‘no maternal milk available’ (NMMA)
-
if insufficient MBM at 48 hr of life to meet requirements, give all available MBM and use appropriate alternative milks to commence or advance feeds
-
Donor breast milk (DBM)
- DBM should be offered to all babies <32 weeks or <1500 g to establish enteral feeds when MBM is unavailable or insufficient to meet baby’s requirements
- DBM may also be offered for the short-term support of any baby on NNU whose mother is seeking to establish breast milk supply
- Essential to add breast milk fortifier (BMF) to DBM to meet nutrient requirements for preterm babies when volume intakes reach 100 mL/kg/day, then advance to 165 mL/kg/day as tolerated
- DBM use is generally restricted to establishing enteral feeds only
- Fortified DBM use can be prolonged for ELBW babies (<1000 g) where there is continued shortfall in MBM, with close monitoring of all growth parameters. Introducing alternative feeds when baby reaches 1000 g or shows suboptimal growth
- Once full volumes achieved (165 mL/kg/day) and baby aged ≥14 days introduce suitable alternative feed based on nutritional requirements (see Slow change to a different type of milk feed)
- Consent for DBM use must be obtained from parents
Breast milk fortifier
- Required by all babies born <34 weeks and/or <1.8 kg fed exclusively on M/DBM to meet protein and micronutrient requirements for growth
- Add BMF when M/DBM volumes reach 100 mL/kg/day
- Increase volume of M/DBM + BMF to maintenance full feeds of 165 mL/kg/day
- Use at full strength in M/DBM
- BMF use should continue until term age
Table 3
|
Nutriprem HMF |
1 sachet HMF added to 25 mL M/DBM |
|
SMA BMF |
1 sachet BMF added to 25 mL M/DBM |
- Prepare as per manufacturer’s instructions:
- add BMF as close to feed time as possible
- swirl breast milk gently to dissolve BMF to protect fragile cellular components in breast milk
- Feed immediately or store in fridge until required and use within 12 hr of preparation
- If baby receiving >50% requirements as preterm formula, stop BMF – unless advised to continue by neonatal dietitian
Table 4: Composition of mother’s own breast milk, and fortified breast milk/100 mL
|
|
Mature breast milk (>2 wk) |
Fortified mature breast milk (Nutriprem HMF) (2021 data card) |
Fortified mature breast milk (SMA PRO BMF) (2020 data card) |
|
Energy (kcal) |
69 |
86 |
86.2 |
|
Protein (g) |
1.3 |
2.6 |
2.74 |
|
CHO (g) |
7.2 |
8.7 |
8.5 |
|
Fat (g) |
4.1 |
4.8 |
4.82 |
|
Sodium (mmol) |
0.7 |
2.9 |
2.35 |
|
Calcium (mmol) |
0.55 |
2.3 |
2.75 |
|
Phosphorus (mmol) |
0.5 |
1.8 |
1.9 |
|
Vitamin A (microgram) |
57 |
289 |
438 |
|
Vitamin D (iU) |
2 |
221 |
<160 |
|
Iron (mg) |
0.07 |
0.07 |
1.87 |
- Use of BMF post discharge is recommended in babies:
- discharged
- establishing oral breast feeding
- showing slow growth velocity
- See for guidance on use of fortifier supplements for babies establishing oral feeds. All babies should be weaned off fortifier supplements by 6 weeks post-term
Table 5: Preparation and administration of fortfier supplements
|
Fortifier breast milk supplements in breast fed babies <40 weeks |
||
|
Nutriprem HMF |
2 sachets HMF added to 3 mL MBM |
Give immediately before a breast feed 4 times per day |
|
SMA BMF |
2 sachets BMF added to 3 mL MBM |
Give immediately before a breast feed 4 times per day |
Protein supplement (Nutriprem protein supplement)
- Use only under direction of neonatal/paediatric dietitian
- Provides extra protein to meet requirements of babies <1000 g
- Indicated if energy and protein intake are below requirements
- Extensively hydrolysed protein alone – NO micronutrients or energy
- Add to M/DBM alongside BMF or direct to preterm formula
- 1 g sachet = 0.82 g protein
- If blood urea in normal range do not add protein supplement discuss with neonatal/paediatric dietitian
- Monitor blood urea twice weekly in all babies on protein supplement
- Stop protein supplement when urea level >6 or when baby reaches 1000 g
Preterm milk formula
- Nutriprem 1/SMA Gold Prem 1: formulated to meet the nutrient needs of preterm babies born <34 weeks or <1.8 kg where insufficient MBM to meet requirements
- Nutriprem 2/SMA Gold Prem 2: nutrient enriched post-discharge formula (NEPDF) formulated to meet the ongoing enhanced nutrient needs of babies born <34 weeks, once beyond term age
- Babies with normal growth velocity and no requirement for catch-up growth may be discharged on term formula with appropriate vitamin and mineral supplementation
- NEPDF especially useful for babies who have higher nutritional requirements (e.g. CLD on oxygen) or babies who have ongoing poor growth (e.g. have crossed down >2 centiles on growth chart during neonatal stay)
- Volumes >165 mL/kg are not usually necessary and other reasons for poor growth should be sought before further volume increases introduced (see Inadequate growth)
Specialised preterm formula (Hydrolysed Nutriprem 1)
- Always use under direction of paediatric/neonatal dietitian
- Hydrolysed Nutriprem 1 – extensively hydrolysed protein preterm formula
- may be suitable for babies who fail to tolerate/progress on standard preterm formula or have a family history of CMPI (NOTE contains lactose)
Table 6: Composition of preterm formula/100 mL
|
Nutriprem 1 (2020 data card) |
Hydrolysed Nutriprem 1 (2020 data card) |
SMA Gold Prem 1 (2020 data card) |
|
| Recommended volumes mL/kg/day | 150–180 | 150–180 | 150 |
| Energy (kcal) | 80 | 80 | 80 |
| Protein (g) |
2.7 (whole protein) |
2.6 (partially hydrolysed) |
2.9 (partially hydrolysed) |
| CHO (g) | 8.4 (55% lactose) | 8.4 (46% lactose) | 8.1 (45% lactose) |
| Fat (g) | 3.9 (8% MCT) |
4 (7% MCT) |
4 (12.5% MCT) |
|
Sodium (mmol) |
3 | 3.3 | 2.4 |
| Calcium (mmol) | 2.5 | 2.4 | 3.0 |
| Phospohorus (mmol) | 2.0 | 1.75 | 2.5 |
| Vitamin A (microgram RE) | 366 | 366 | 330 |
| Vitamin D (microgram) | 3.1 | 3.1 | 3.4 |
All 'specialised' term formulas
- Do not provide adequate nutrition for preterm babies at standard dilution so require modification to ensure nutritional requirements met. Use only when clinically indicated and always under direction of paediatric/neonatal dietitian
Table 7: Maintenance feeds based on gestational age and/or weight
|
Gestational age and/or weight |
Maintenance feed |
|
<32 weeks and/or <1000 g |
|
|
Born between or on reaching 32+1–33+6 weeks |
|
|
On reaching 34 weeks
|
|
|
Preterm babies (born <34 weeks) at discharge or term age (whichever is earliest)
|
<36+6 weeks
≥37 weeks
|
|
Born ≥34–37 weeks and <1.8 kg |
|
|
Born ≥34 weeks and ≥1.8 kg |
|
Change to different type of milk feed
- Done slowly to ensure baby tolerates change
- Day 1: 75% feeds with current milk, 25% with new milk (i.e. 3 old feeds:1 new feed)
- Day 2: 50% feeds with current milk, 50% with new milk (i.e. 2 old feeds:2 new feeds)
- Day 3: 75% feeds with new milk, 25% with current milk (i.e. 1 old feed:3 new feeds)
- Day 4: 100% new milk
- It is acceptable to mix the milks together
VITAMIN SUPPLEMENTATION
- Start enteral vitamin supplements when baby reaches 100 mL/kg/day enteral feeds
- For baby transitioning from PN start enteral vitamins when on 10 mL/kg/day lipids
- Continue vitamin doses until aged 6 months corrected – then follow Department of Health baby vitamin supplementation guidelines
Table 8
| Current weight | Choose ONLY 1 multivitamin preparation | Folic acid | |||
| ABIDEC | Healthy start vitamins | DALIVIT | |||
| Babies born <34 weeks and /or <1.8 kg | |||||
|
Fortified MBM/DBM Preterm formula (Nutriprem 1 or SMA Gold Prem 1) |
≤1 kg | 0.3 mL once daily | 3 drops once daily |
X Vitamin D only Colecalciferol 200 units daily |
X |
| >1 kg | 0.6 mL once daily | 5 drops once daily |
X Vitamin D only Colecalciferol 400 units daily |
X | |
| *Unfortified MBM/DBM | ≤1 kg | 0.6 mL once daily | 5 drops once daily | 0.3 mL once daily and Vitamin D Colecalciferol 200 units daily |
50 microgram once daily |
| >1 kg | 0.6 mL once daily and vitamin D Colecalciferol 600 units alternate days | 5 drops once daily and vitamin D Colecalciferol 600 units alternate days | 0.3 mL once daily and vitamin D Colecalciferol 600 units daily |
50 microgram once daily |
|
| Choose ONLY 1 multivitamin preparation | Folic acid | ||||
| ABIDEC | Healthy start vitamins | DALIVIT | |||
| Babies born <34 weeks’ gestation when reaching ≥1.8 kg | |||||
|
Post discharge formula (Nutriprem 2/SMA Gold 2) MBM and post-discharge fortifier High energy infant formula (Infatrini/SMA high energy) |
0.3 mL once daily | 3 drops once daily |
X Vitamin D only Colecalciferol 200 units daily |
X | |
|
Unfortified MBM Term formula |
0.6 mL once daily | 5 drops once daily | 0.3 mL once daily and vitamin D Colecalciferol 200 units daily | X | |
*Preterm babies fed exclusively on unfortified breast milk will not meet recommended intakes for calcium/phosphate and other essential micronutrients. Care needs to be taken to ensure risk of deficiency of micronutrients is minimised, especially the impact on metabolic bone disease (see Metabolic bone disease guideline for advice on screening and supplementation)
† NOTE doses of ABIDEC® and DALIVIT® are not equivalent due to differing levels of vitamin content, especially vitamin A. In the absence of ABIDEC consider using Healthy Start Vitamins as next best alternative or seek advice of neonatal dietitian/pharmacist (see Table 9 below)
Table 9: Multivitamin supplements
| Abidec 0.6 mL | Dalivit 0.6 mL |
Healthy start children's vitamin 5 drops |
|
| Vitamin A (units) | 1333 | 5000 | 776 |
| Vitamin D (units) | 400 | 400 | 400 |
| Vitamin C (mg) | 40 | 50 | 20 |
| Thiamine B1 (mg) | 0.4 | 1 | X |
| Riboflavin B2 (mg) | 0.8 | 0.4 | X |
| Pyridoxine B6 (mg) | 0.8 | 0.5 | X |
| Nicotinamide B3 (mg) | 8 | 5 | X |
IRON SUPPLEMENTATION
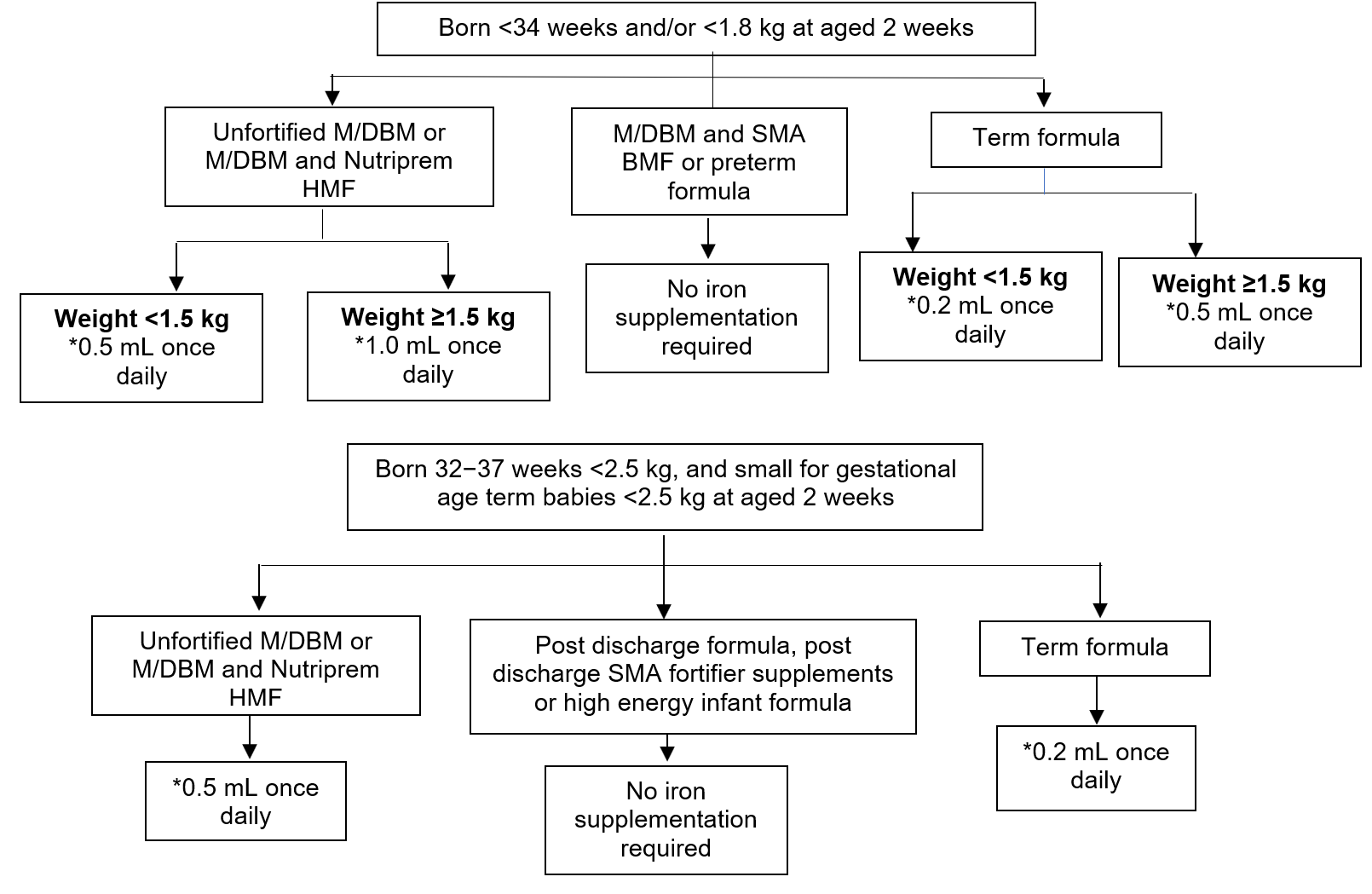
- Only required where milk feed does not contain enhanced iron levels to meet recommended intakes – see Flowchart 2
- Start iron supplementation from aged 2 weeks and tolerating 100 mL/kg/day enteral feeds
- note: in babies not tolerating 100 mL/kg/day enteral feeds at aged 2 weeks discuss administration of iron supplements with neonatal dietitian or pharmacist
- Using *sodium feredetate (27.5 mg iron per 5 mL)
- Recommended iron intakes − see Table 10
Table 10
| Baby | Birth weight | Iron intake, AIM: |
| Preterm <34 weeks | <1.8 kg | 2−3 mg/kg/day |
| ≥34−<37 weeks | <2 kg | 2−3 mg/kg/day |
| Term baby ≥37 weeks | 2–2.5 kg | 1−2 mg/kg/day |
- Continue iron supplements until aged 12 months corrected age
- Monitor iron intake by regular measurements of Hb, serum ferritin and CRP
Flowchart 2: Iron supplementation to meet recommended intakes
FEED TOLERANCE EVALUATION
Monitoring of feed tolerance, growth and biochemical balance is critical in nutritional management of preterm babies to ensure optimal outcomes
Feed tolerance
- Poor gut motility is common among VLBW/ELBW babies, and some will have episodes requiring temporary discontinuation of feeding or delay in advancing feeds
- If failure to progress feeds continues over several days, seek advice early from neonatal/paediatric dietitian
Assessment of gastric residuals (GR)
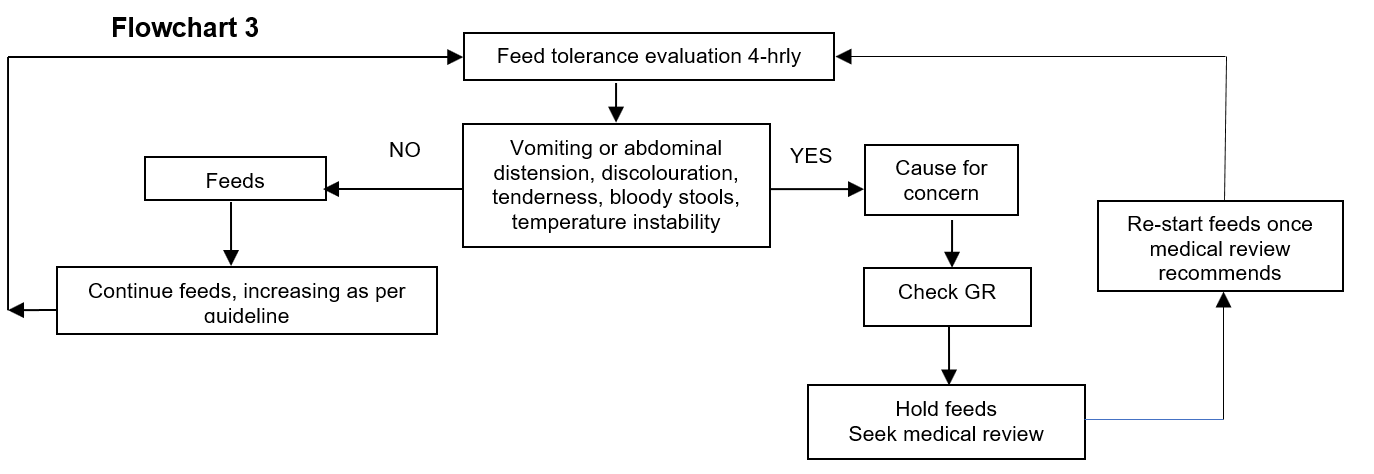
- Evaluate feed tolerance 4-hrly (see Flowchart 3)
- Routine aspiration of GR not recommended in preterm babies
- Do not use GR volumes in isolation when deciding to limit advancement of feeds
Flowchart 3
Anthropometry
- See Growth monitoring guideline
Biochemical monitoring
- Measure plasma urea, electrolytes, ALP, calcium, and phosphate weekly in stable preterm babies
- Monitor glucose closely in initial few days
INADEQUATE GROWTH VELOCITY
- Preterm babies with suboptimal growth velocity require further assessment
- Review proportional growth (weight, head, length) on age and gender appropriate growth chart
- Ensure baby prescribed and receiving recommended nutritional intake. Ensure on maximum advised volume of age/weight appropriate feed – see maintenance feed volume/type charts
- Review energy and protein intake per kg/day against ESPGHAN recommendations for weight/gestation
- Measure urine sodium concentration. Value <20 mmol/L indicates sodium depletion (not valid if baby on diuretics)
- If sodium supplements required:
- check urine sodium weekly
- keep total enteral sodium intake (feed + standard supplement + prescribed supplement) <8 mmol/kg/day
- In babies receiving MBM use hind milk (see Breast milk expression guideline)
- Check zinc level in cases of poor growth associated low ALP, especially in surgical babies where excess GI losses are possible and supplement if low
- Refer to neonatal/paediatric dietitian for assessment and advice
- Do not advance feed volumes beyond that recommended unless on advice of dietitian
- Formula fed >37 weeks, ≥2 kg:
- replace 25–50% MBM/NEPDF with high energy term formula (Infatrini, SMA® High Energy, Similac® High Energy) and refer to paediatric/neonatal dietitian for follow-up
- Breast milk fed >37 weeks:
- stop any BMF in MBM but continue with concentrated BMF supplements as detailed in Breast milk fortifier section
Exclusively breastfed babies should receive vitamin D supplementation from birth