DEFINITION
Congenital anomaly with blind ending oesophagus which may be associated with a fistula between the abnormal oesophagus and the trachea
DIAGNOSIS
- Suspect antenatally if scans show polyhydramnios +/- absent stomach bubble
- refer to fetal medicine specialist
- plan appropriate place of delivery
- parents should meet paediatric surgeon antenatally
- Most cases present shortly after birth. Suspect if:
- history of polyhydramnios +/- absent stomach bubble
- frothing at mouth
- respiratory symptoms on feeding
- difficulty in passing nasogastric tube (NGT)
- anorectal malformation (see Anorectal malformation guideline)
DELIVERY
- If diagnosis suspected antenatally, avoid:
- any positive pressure ventilation [including mask ventilation, HFNC, CPAP and endotracheal tube (ETT)]; pouch
- distension may lead to respiratory compromise and/or aspiration via a distal pouch fistula
- If intubation indicated, ETT tip as close to carina as possible to minimise gas flow through a fistula. Ventilatory pressures should be as low as possible
- If any significant respiratory compromise, instigate a time critical transfer to surgical unit
- if transferring to BCH call KIDS NTS (will conference call surgeons and PIC)
Confirmation of diagnosis
- Experienced operator to place radio-opaque 8 Fr NGT. Typically resistance is felt 10–12 cm from nostril in term baby
- do not use force (may lead to oesophageal perforation)
- AP X-ray of whole chest and abdomen
- diagnosis confirmed if NGT curled in upper oesophagus
- gastric air bubble/bowel gas confirms presence of fistula between trachea and distal oesophagus
- Do not attempt a contrast oesophagogram
MANAGEMENT ON NNU
- If respiratory support required or abdominal distension, contact surgical unit and transfer team immediately (time critical transfer)
- Nurse 30° head-up with head turned to side to facilitate drainage of secretions
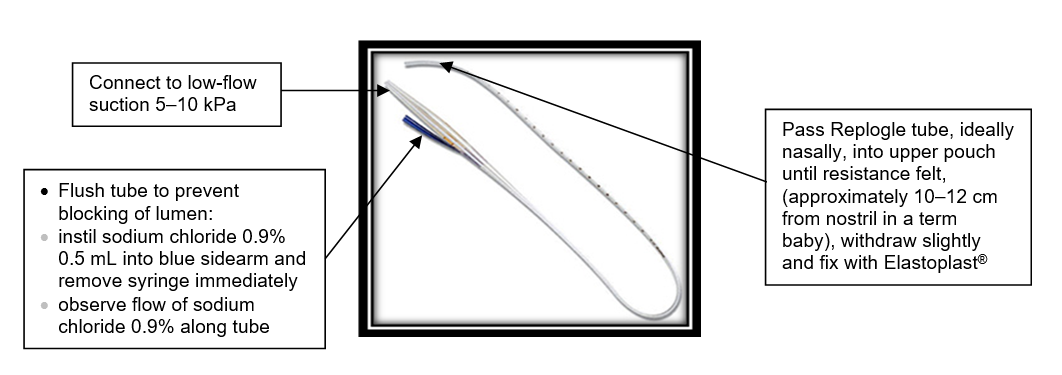
- Pass 10 Fr Replogle tube into oesophageal pouch (see Insertion and management of Replogle tube)
- if Replogle tube unavailable, place 10 Fr NGT into pouch, aspirating every 15 min
- an NGT cannot be placed on suction so needs regular, intermittent aspiration
- Insert until resistance is met, then withdraw by 1 cm
- Tape securely to face. Usually 10–12 cm at nostril in a term baby
- Place mittens on baby to prevent tube being pulled out
- Attach tapered end of tube to continuous low flow suction. Start pressure at 5 kPa aiming for continuous flow of secretions from upper oesophagus. Maximum pressure 10 kPa
- do not share suction with other drains e.g. chest drain
- Baby should be relaxed and pink with no respiratory distress or secretions in the mouth
- Keep nil-by-mouth
- Flush Replogle tube with sodium chloride 0.9% 0.5 mL via the sidearm every 15 min. More frequently if visible oral secretions
- If using an enteral tube to drain saliva, aspirate every 15 min, more frequently if visible oral secretions or respiratory difficulty evident
- If no movement of secretions in Replogle tube after flushing with sodium chloride 0.9% 0.5 mL via the sidearm, change tube
- Do not leave syringe attached to sidearm as this will prevent the tube working effectively
- change tube every 10 days, or daily if viscous secretions
Samples
- Obtain IV access
- Take blood for FBC, clotting, U&E, blood glucose and blood culture
- Birmingham Children’s Hospital do not require a baby crossmatch sample before transfer
- Send 1 bloodspot on neonatal screening card to surgical unit with baby for sickle cell screening (mark card 'pre-transfusion')
Fluids and medication
- Commence maintenance IV fluids (see Intravenous fluid therapy guideline)
- Give vitamin K IM (see Vitamin K guideline)
- Start broad spectrum antibiotics IV (see Neonatal Formulary)
Referral
- Examine baby for other associated abnormalities (e.g. cardiac murmur, anorectal abnormalities). If major congenital abnormality detected, discuss with consultant before arranging transfer for management of oesophageal atresia as this may not be appropriate
- Discuss baby’s condition and treatment plan with parents and ensure they have seen baby before transfer. Take photographs for parents
- Contact surgical centre to arrange transfer as soon as possible
- Obtain sample of mother’s blood for crossmatch
- sample tube must be clearly hand written and labelled with mother’s name, date of birth, NHS number, and date and time of collection
- complete form
- add baby’s details to ensure it is clear sample relates to mother of baby being transferred (this information is required by surgical unit blood bank)
- Complete nursing and medical documentation for transfer and send copies of X-rays by PACS. Ensure you have mother’s contact details (ward telephone number or home/mobile number if she has been discharged). Surgeon will obtain verbal telephone consent if operation is required and an individual with parental responsibility is not able to attend surgical unit at appropriate time
- Inform surgical unit staff when baby is ready for transfer. Have available: name, gestational age, weight, ventilatory and oxygen requirements (if applicable) and mother’s name and ward (if admitted)
Insertion and management of Replogle tube
AIM
To prevent aspiration of secretions by continuous drainage of upper oesophageal pouch
Equipment
- Replogle tube size 10 Fr + 1 spare to keep at bedside
- Low-flow suction
- Regular suction
- 2 mL IV syringe
- Sodium chloride 0.9%
- Duoderm® dressing and Elastoplast®
- Lubricant
Monitoring
- Check Replogle tube several times an hour and flush to prevent blocking of lumen by instilling sodium chloride 0.9% 0.5 mL into blue sidearm, removing syringe immediately and observing the flow of secretions along the tube. Monitor oxygen saturation, respiratory status and heart rate continuously
- For long-term Replogle use, monitor electrolytes and consider replacement therapy
Blocked tube
- Suspect if:
- no continuous flow of secretions along tube
- visible oral secretions
- baby in distress
- Clear airway with high-flow oropharyngeal suction
- Increase low-flow suction and flush Replogle tube with air, observing flow of saliva along tube
- If patency not restored, replace with new Replogle tube and return low-flow suction to previous level
- If Replogle tube replaced, alternate nostrils to avoid long-term stretching of nares
USEFUL INFORMATION
Date updated: 2024-02-08